Safe Opioid Reduction: How to Taper Off Opioids Safely and What Works
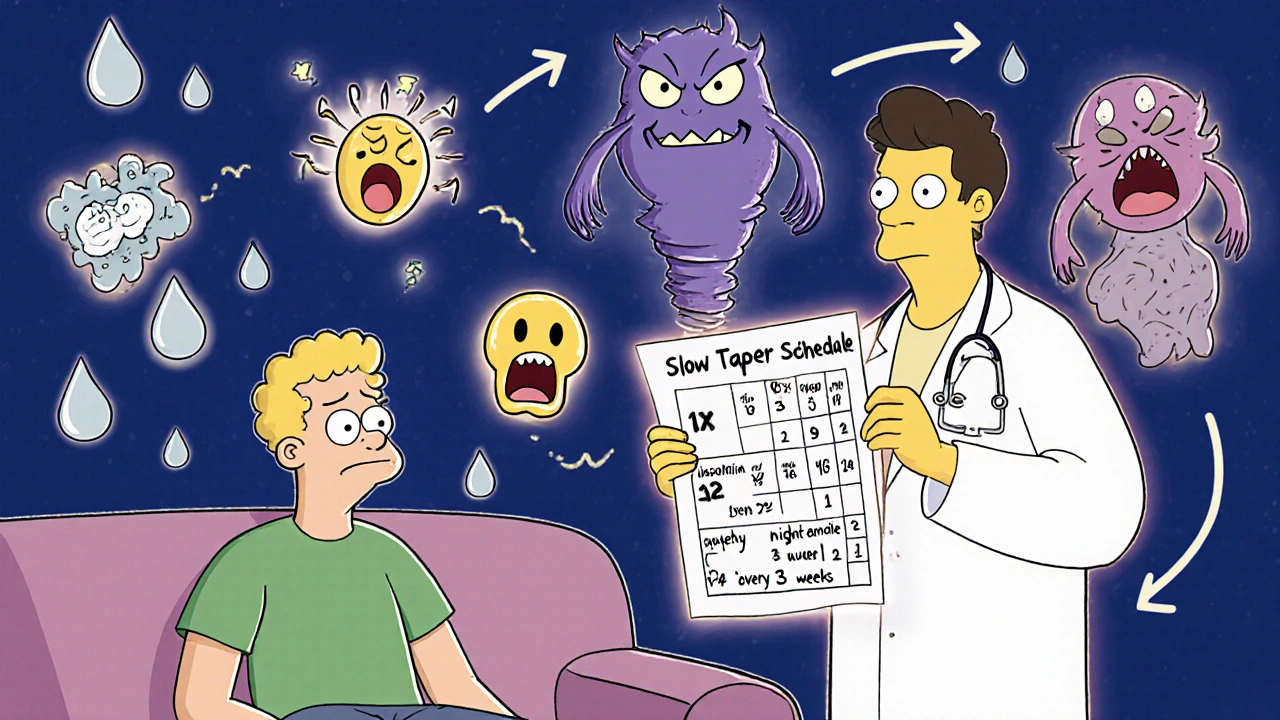
When you’ve been taking opioids for pain, stopping isn’t just about quitting a drug—it’s about safe opioid reduction, a planned, gradual process to lower dosage without triggering severe withdrawal or rebound pain. Also known as opioid tapering, it’s not a one-size-fits-all fix. Many people try to quit cold turkey and end up back on the medication—or worse, in crisis. The goal isn’t speed. It’s sustainability.
Successful opioid tapering, a step-by-step decrease in opioid dosage under medical supervision. Also known as opioid dose reduction, it requires patience and support isn’t just about cutting pills. It’s about replacing the physical reliance with better pain control and emotional tools. That’s why pain management, a holistic approach to reducing discomfort without over-relying on opioids. Also known as non-opioid pain relief, it includes physical therapy, nerve blocks, and even cognitive behavioral techniques plays such a big role. You can’t just remove the opioid and hope your body figures it out. You need alternatives that actually work. And you need to know what’s normal—like mild anxiety or trouble sleeping—versus what’s dangerous, like rapid heartbeat or extreme confusion. That’s where understanding withdrawal symptoms, the physical and emotional reactions your body has when opioids are reduced too fast. Also known as opioid withdrawal, these include nausea, muscle aches, and insomnia helps you stay calm and stick to your plan.
Some people think tapering means going slower and slower until you’re off. Others think they need to switch to a different opioid first. Neither is always right. The best approach depends on how long you’ve been taking the drug, your dose, your health, and your mental state. That’s why you’ll find real stories here—not theory. Posts cover how people managed side effects while cutting back, what worked when pain came back, and how some used non-opioid meds like gabapentin or low-dose antidepressants to help. You’ll also see how medication safety, the practice of using drugs in a way that minimizes harm and maximizes benefit. Also known as drug safety, it includes tracking interactions, avoiding overdose, and knowing when to call your doctor ties into every step: storing pills securely, not mixing with alcohol, recognizing when a symptom needs urgent care.
There’s no magic pill for quitting opioids. But there are proven steps, real experiences, and tools that make the path less lonely. What follows isn’t a checklist. It’s a collection of practical, honest guides written by people who’ve been there—whether they tapered over months or needed to adjust their pain plan after surgery. You’ll find what to expect, what to avoid, and how to keep going when it feels impossible. This isn’t about willpower. It’s about smart, safe choices—and the resources to make them.
Tapering Opioids Safely: How to Reduce Side Effects and Avoid Withdrawal
Learn how to safely reduce opioid use with a slow, personalized taper to avoid severe withdrawal and dangerous side effects. Evidence-based strategies for managing pain and improving quality of life.
