Opioid Tapering Calculator
Tapering Information
Calculate your personalized opioid tapering schedule based on CDC guidelines and your current medical situation.
Your Tapering Schedule
Why Tapering Opioids Isn’t Just About Cutting Doses
Many people think tapering off opioids means simply taking less each day until you stop. That’s not true-and it can be dangerous. Abruptly stopping opioids after long-term use can trigger severe withdrawal, worsen pain, or even lead to suicide. The opioid tapering process isn’t a one-size-fits-all checklist. It’s a personalized plan built on your health history, pain levels, mental state, and how your body reacts to changes.
Between 2017 and 2020, 12% of primary care providers mistakenly stopped opioids cold turkey for stable chronic pain patients, thinking they were following guidelines. That mistake led to at least 17 documented suicides. The CDC updated its guidelines in 2022 to make this crystal clear: rapid tapering increases overdose risk by 68% and suicide attempt risk by 78%. This isn’t just a medical issue-it’s a safety issue.
When Is Tapering Actually Needed?
You don’t taper opioids just because you’ve been on them for a while. There are clear medical reasons to consider reducing your dose:
- You’re not getting better pain relief-even at higher doses
- You’re experiencing serious side effects like drowsiness, confusion, constipation, or trouble breathing
- You’ve had an overdose or near-overdose
- You’re using opioids along with benzodiazepines (like Xanax or Valium), which increases overdose risk
- You’re refilling prescriptions early, losing pills, or getting them from multiple doctors
- You’re showing signs of depression, anxiety, or suicidal thoughts
If any of these apply, it’s time to talk to your doctor-not panic and quit on your own.
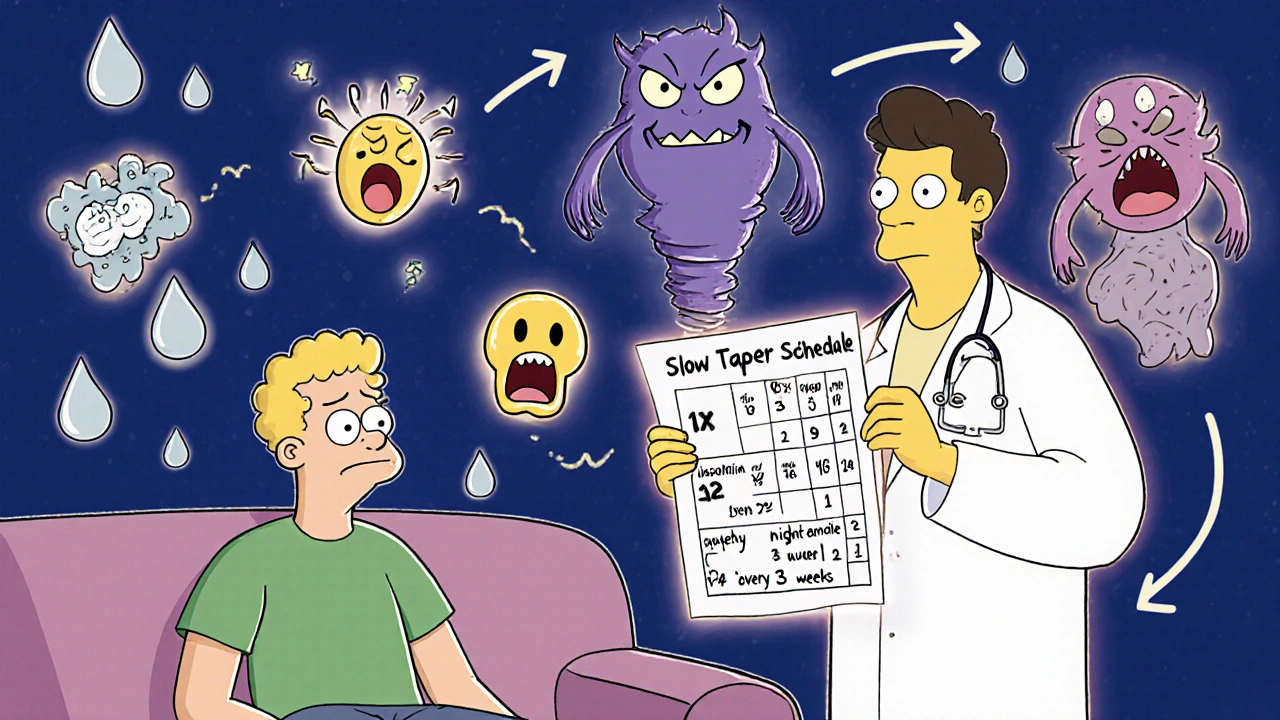
The Right Speed: Slow Is Safer Than Fast
There’s no magic number for how fast to taper. But research gives us hard truths:
- Fast taper: Cutting more than 10% per week. This is risky. It triggers severe withdrawal and increases overdose risk.
- Slow taper: Cutting 10-25% every 2-4 weeks. This is the standard for most people.
- Very slow taper: 5-10% per month. This is for people on very high doses (>120 MME daily), those with trauma history, or complex mental health conditions.
A 2022 survey of 1,200 chronic pain patients found that 63% preferred a 10% monthly reduction. Those people stuck with their taper 32% longer than those who tried faster cuts. Why? Because their bodies had time to adjust.
Here’s how a typical slow taper might look:
- Reduce your daily dose by 10-20% every 3 weeks
- Keep your nighttime dose until last-it helps with sleep and pain control
- Don’t reduce frequency before dose. If you take it three times a day, cut the amount per dose first
- After reaching 30% of your original dose, slow down even more: 5% every 2-4 weeks
Some people stabilize at a low maintenance dose (like 20-30 MME daily) and never fully stop. That’s okay. The goal isn’t always zero-it’s better function and fewer side effects.

What Happens During Withdrawal (And How to Manage It)
About 35% of people on long-term opioids experience moderate to severe withdrawal during tapering. Symptoms aren’t just uncomfortable-they can be debilitating:
- Anxiety (82% of people report this)
- Insomnia (76%)
- Muscle aches and cramps (68%)
- Diarrhea, nausea, vomiting (59%)
- Sweating, chills, runny nose
- Increased pain sensitivity (hyperalgesia)
You don’t have to suffer through this alone. Supportive medications can help:
- Clonidine (0.1-0.3 mg twice daily): Reduces sweating, anxiety, high blood pressure, and rapid heartbeat
- Hydroxyzine (25-50 mg at bedtime): Helps with anxiety and sleep
- Loperamide (2-4 mg as needed): Controls diarrhea
- NSAIDs or acetaminophen: For pain that returns as opioids drop
These aren’t addictive. They’re tools to make the process bearable. Your doctor can prescribe them alongside your taper.
Never Taper Alone: The Role of Support and Planning
One of the biggest predictors of success? Patient agreement. If you’re forced into a taper, you’re more likely to quit it-or relapse. The CDC found tapers with patient buy-in had 47% lower discontinuation rates.
That’s why shared decision-making is now the gold standard. Before you start:
- Review your medical records with your doctor
- Discuss your pain goals: Is it to walk without help? Sleep through the night? Return to work?
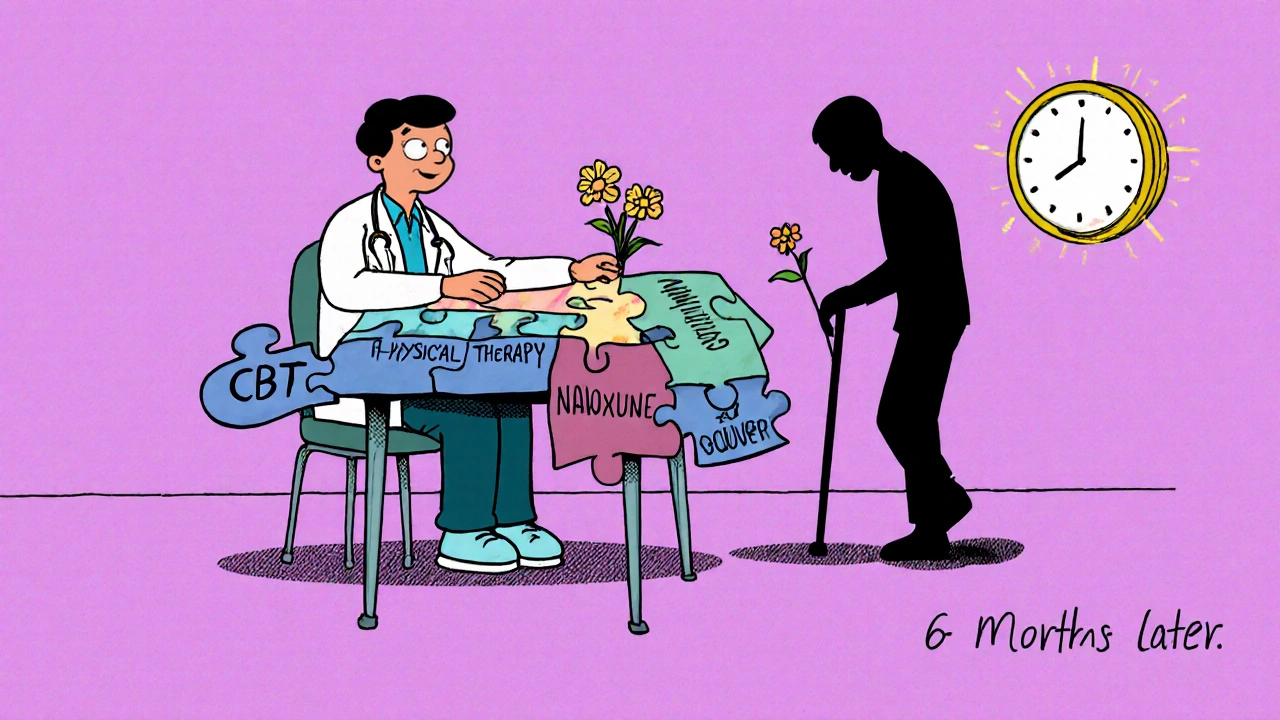
- Ask about non-opioid options: physical therapy, CBT, acupuncture, nerve blocks
- Sign a written tapering agreement (87% of successful tapers include one)
Also, get naloxone. The Substance Abuse and Mental Health Services Administration (SAMHSA) recommends it for anyone tapering with a history of overdose, high doses (>50 MME), or use of benzodiazepines. Why? Forty-one percent of overdoses during tapering happen in the first 30 days. Naloxone can save your life.
What to Do If Your Pain Gets Worse
It’s common for pain to feel worse during tapering. Your nervous system has adapted to opioids. When you reduce them, your body overreacts. This isn’t your pain returning-it’s your nerves being hypersensitive.
Here’s how to handle it:
- Don’t go back to your old dose. That resets your progress.
- Use non-opioid pain relief: heat packs, gentle movement, massage, meditation
- Ask your doctor about gabapentin or pregabalin for nerve pain
- Consider cognitive behavioral therapy (CBT)-it helps retrain how your brain processes pain
- Physical therapy can rebuild strength and reduce reliance on pills
Studies show patients who combined tapering with CBT and physical therapy cut their failure rate in half-from 44% down to 19% in six months.
Red Flags: When Tapering Is Too Risky
Some people shouldn’t taper without extra support:
- Active opioid use disorder
- Untreated depression, PTSD, or anxiety
- History of suicide attempts or self-harm
- Current use of benzodiazepines or alcohol
- Very high doses (>120 MME daily)
If any of these apply, you need more than a taper. You need a team: a pain specialist, a mental health provider, and possibly medication-assisted treatment (MAT) with buprenorphine. Buprenorphine helps reduce cravings and withdrawal without the same overdose risk as full opioids.
What Happens After You Finish?
Stopping opioids doesn’t mean your pain journey ends. Many people find their pain improves over time as their nervous system resets. Others learn to manage it differently.
After tapering:
- Keep your doctor appointments for at least 6 months
- Track your pain and function in a journal
- Stay active-even light walking helps
- Use mindfulness or breathing techniques to manage flare-ups
- Join a support group for people who’ve tapered off opioids
Remember: 68% of successful tapering plans focus on improving function, not just eliminating pills. Walking to the mailbox, sleeping through the night, playing with your kids-those are real wins.
Final Reminder: You’re Not Alone
Tapering opioids is one of the hardest things you’ll do for your health. It takes time, patience, and support. You don’t have to do it alone. There are doctors, therapists, and peer groups ready to help. And if your current provider pushes you to cut too fast? Get a second opinion. Your safety matters more than any guideline.
The goal isn’t to be opioid-free at all costs. It’s to live better-with less pain, fewer side effects, and more control over your life.
Can I taper off opioids on my own?
No. Tapering opioids without medical supervision is dangerous. Withdrawal symptoms can be severe, and sudden discontinuation increases the risk of overdose, suicide, and uncontrolled pain. Always work with a doctor who understands opioid tapering guidelines.
How long does opioid withdrawal last?
Acute withdrawal symptoms usually peak within 72 hours after the last dose and can last 1-2 weeks. Some symptoms like anxiety, insomnia, and pain sensitivity can linger for weeks or months. This is called post-acute withdrawal syndrome (PAWS). Slow tapering helps reduce the severity and duration of these symptoms.
Will my pain get worse after I stop opioids?
It’s common for pain to feel worse temporarily as your body adjusts. This is called opioid-induced hyperalgesia. Over time, many people find their pain improves, especially when combined with physical therapy, CBT, or other non-opioid treatments. The key is not to go back to opioids-stick with the plan and give your nervous system time to reset.
What medications help with opioid withdrawal symptoms?
Clonidine helps with sweating, anxiety, and high blood pressure. Hydroxyzine improves sleep and anxiety. Loperamide controls diarrhea. NSAIDs or acetaminophen can manage residual pain. These are not addictive and are often prescribed alongside tapering to make it more manageable.
Is it safe to taper if I’m on high doses?
Yes-but it must be done slowly and with support. People on doses over 120 MME daily need extra care. A very slow taper (5-10% per month) is recommended. You may also need mental health support, naloxone, or medication-assisted treatment like buprenorphine. Never rush a high-dose taper.
What if my doctor wants me to taper too fast?
Ask for evidence. Cite the CDC’s 2022 guideline, which warns against rapid tapering. You have the right to a plan you can follow. If your doctor won’t adjust, seek a second opinion from a pain specialist or addiction medicine provider. Your safety comes first.

Comments
Iska Ede
November 18, 2025 AT 17:18Meanwhile, my cousin tapered off fentanyl in 3 weeks with a yoga mat and a dog named Biscuit. He’s now running marathons. Guess the CDC doesn’t know about Biscuit.
Gabriella Jayne Bosticco
November 20, 2025 AT 16:46And yeah - my pain’s still there sometimes. But now I’m living with it, not drowning in it.
Sarah Frey
November 21, 2025 AT 12:04Furthermore, the integration of non-pharmacological modalities - including cognitive behavioral therapy and physical rehabilitation - demonstrates statistically significant improvements in functional outcomes, as corroborated by longitudinal cohort studies published in JAMA Pain Medicine.
Katelyn Sykes
November 22, 2025 AT 03:57Clonidine was a game changer honestly it took the worst of the shakes away
Also started swimming and my pain actually got better over time like my body finally stopped screaming for the drug
And yes I still take 25 MME now and I dont care its not about zero its about not being a zombie
Gabe Solack
November 24, 2025 AT 01:50My brother tapered slowly with buprenorphine and now he’s coaching little league. No more nodding off at dinner. No more hiding pills. Just… him.
Naloxone? Got it. Learned how to use it. Took it to his first game. Felt like a superhero.
Don’t let anyone rush you. You’re not broken. You’re healing.
Yash Nair
November 25, 2025 AT 04:32Bailey Sheppard
November 25, 2025 AT 08:30If you’re reading this and you’re scared - you’re not alone. Take it one day at a time. You’ve already won by showing up.
Girish Pai
November 25, 2025 AT 09:50Kristi Joy
November 26, 2025 AT 13:46Some days will feel impossible. On those days, just breathe. Drink water. Sit outside. You don’t have to fix everything today. Just show up. That’s enough.
I’m proud of you. Even if you don’t feel it yet.
Hal Nicholas
November 28, 2025 AT 08:59Yeah. Right.
He’s lying. Everyone relapses. This whole ‘slow taper’ thing is just a placebo for people who don’t want to face the truth: opioids ruin lives. You either quit cold turkey or you stay a slave. There’s no middle ground. This article is sugar-coating addiction.
Louie Amour
November 29, 2025 AT 16:25Those who ‘taper slowly’ are simply delaying inevitable clinical collapse. This is not medicine - it’s appeasement.
Shaun Barratt
November 29, 2025 AT 21:00