Rare Disease Drugs: What They Are, Who Needs Them, and How They Work
When a condition affects fewer than 200,000 people in the U.S., it’s called a rare disease drug, a medication developed specifically for conditions with very small patient populations, often called orphan diseases. Also known as orphan drugs, these treatments are designed for illnesses that big pharmaceutical companies once ignored because the market was too small to justify the cost. But that changed in the 1980s, when laws like the Orphan Drug Act gave incentives to companies willing to develop them. Today, over 7,000 rare diseases exist—and nearly 60% of them now have at least one approved treatment.
These aren’t just experimental pills. Many rare disease drugs are highly targeted, using advanced science to fix specific genetic errors or block abnormal proteins. For example, a drug might replace a missing enzyme in someone with Gaucher disease or silence a faulty gene causing spinal muscular atrophy. Unlike common meds like ibuprofen or metformin, these treatments often cost tens or even hundreds of thousands of dollars a year. That’s why access is such a big issue—insurance doesn’t always cover them, and patients may wait months just to get approval.
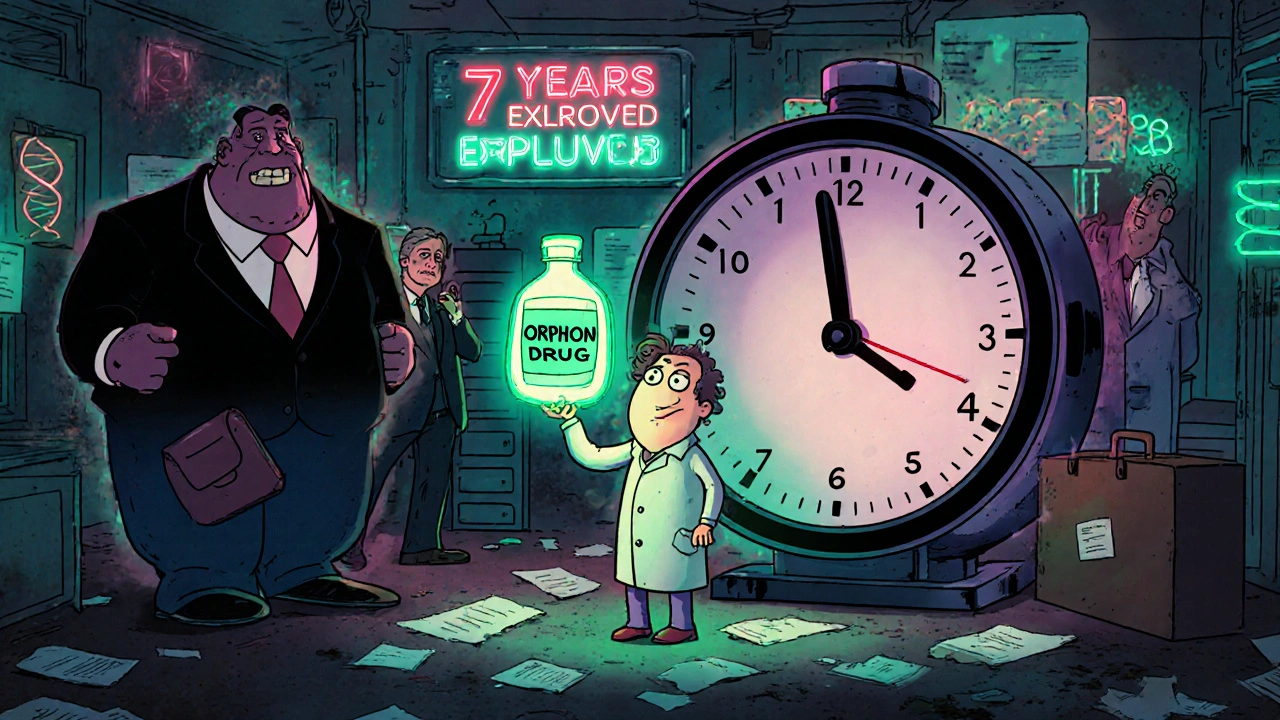
Behind every rare disease drug is a long road: years of research, small clinical trials with just dozens of patients, and complex FDA review. The FDA approval, the process by which the U.S. Food and Drug Administration evaluates whether a new drug is safe and effective for public use for these drugs can be faster than for common medications, thanks to special designations like Breakthrough Therapy or Fast Track. But even with shortcuts, getting a drug to market takes time—and many patients don’t have that time.
Patients and families often become experts overnight. They join advocacy groups, push for research funding, and sometimes even help design clinical trials. The specialty medications, high-cost, complex drugs requiring special handling, monitoring, or administration, often used for chronic or rare conditions used in rare diseases aren’t something you pick up at your local pharmacy. They usually come through specialty distributors, require cold storage, or need nurse training to administer. That’s why some patients rely on organizations that help with insurance appeals, co-pay assistance, or even finding the right doctor.
And while rare disease drugs are a triumph of modern medicine, they’re not perfect. Some work brilliantly for a few, but not everyone responds. Others have serious side effects—like liver damage or immune suppression—that require constant monitoring. That’s why knowing when to push for a new treatment, and when to manage side effects, matters just as much as the drug itself. You’ll find posts here that break down real cases: how clobetasol helps with skin lymphoma, how nimodipine is used long-term, and how patients cope with the emotional weight of taking a drug no one else uses.
What you’ll find below isn’t just a list of articles. It’s a collection of real stories, comparisons, and practical advice from people who live with these conditions—or help treat them. Whether you’re a patient, a caregiver, or just trying to understand why some meds cost more than a car, these posts give you the facts without the fluff. No jargon. No hype. Just what you need to know.
Orphan Drug Exclusivity: How Rare-Disease Medicines Get Market Protection
Orphan drug exclusivity gives pharmaceutical companies seven years of market protection for rare-disease treatments, encouraging development where profits are low. Learn how it works, why it matters, and who benefits.
