Opioid-Induced Adrenal Insufficiency: Causes, Symptoms, and What to Do
When you take opioids long-term, your body can stop making its own stress hormones — a condition called opioid-induced adrenal insufficiency, a hormonal disorder caused by prolonged opioid use that suppresses the adrenal glands’ ability to produce cortisol. It’s not rare, but it’s often missed because the symptoms look like fatigue, depression, or just "being worn out." This isn’t withdrawal — it’s your body’s natural stress response system shutting down because opioids fool your brain into thinking it doesn’t need to make cortisol anymore.
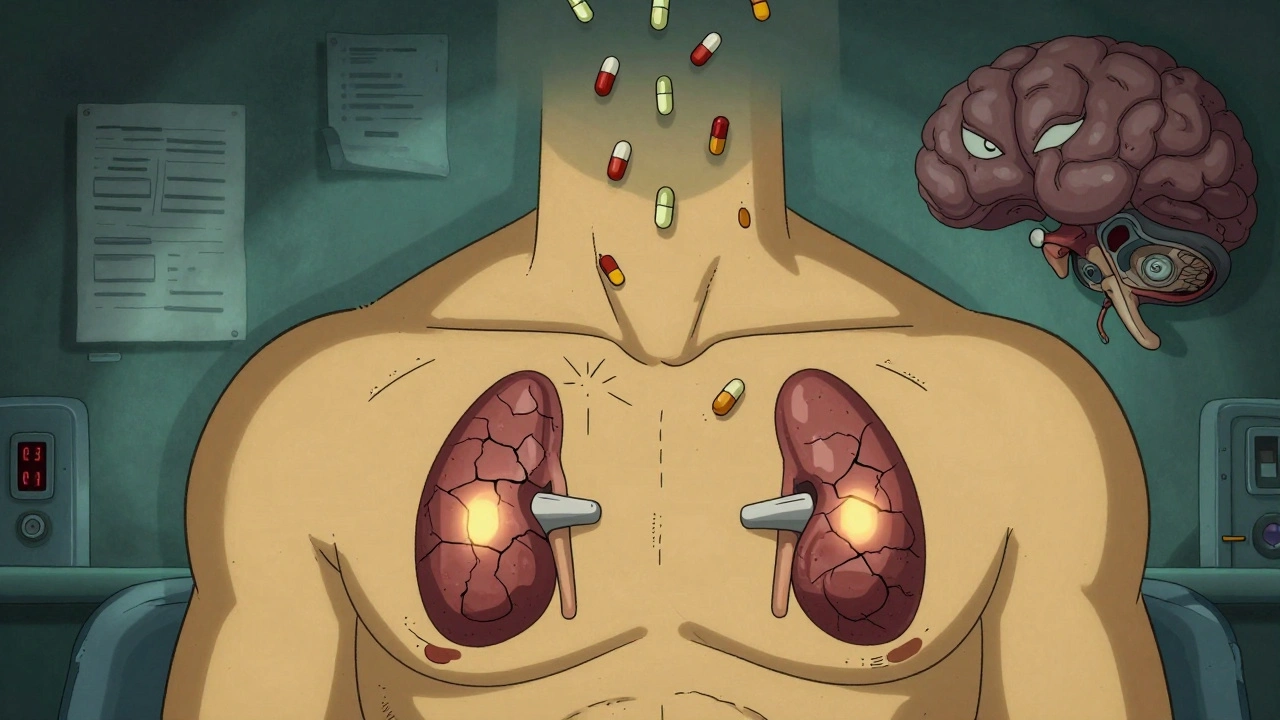
People on high-dose or long-term opioid therapy — especially for chronic pain — are at risk. The adrenal glands, which sit on top of your kidneys, normally release cortisol when you’re stressed, sick, or injured. But opioids block the signals from your brain that tell those glands to work. Over time, they shrink back. When you cut back or stop opioids, your body doesn’t know how to restart cortisol production. That’s when you get dizzy, weak, nauseous, or even pass out — not from pain, but from low blood pressure and low sugar because your body has no stress buffer.
adrenal insufficiency, a condition where the adrenal glands don’t produce enough steroid hormones, especially cortisol can be life-threatening if ignored. Emergency rooms see patients with this condition after surgery, infection, or trauma — they don’t respond to normal treatments because their bodies can’t ramp up cortisol. And here’s the kicker: many doctors don’t test for it unless you’re clearly crashing. If you’ve been on opioids for more than a few months and feel constantly tired, lose your appetite, or get sick easily, ask for a cortisol test. It’s simple: a blood test in the morning, before you take your meds.
steroid withdrawal, the drop in hormone levels that happens when the body stops producing its own steroids after long-term suppression is what you’re dealing with here. It’s not the same as opioid withdrawal, but it can make it worse. You might think your nausea and weakness are from quitting pain meds — but they could be from your adrenals not working. That’s why tapering opioids slowly matters. A slow, guided reduction gives your body time to wake up its own hormone production. Some people need a short course of synthetic cortisol during tapering to avoid collapse.
This isn’t about avoiding opioids. It’s about using them wisely and knowing when your body is paying a hidden price. If you’re on opioids for chronic pain, get checked. If you’re tapering and feel worse instead of better, don’t assume it’s just withdrawal. Ask about cortisol. Bring this up with your doctor — not as a theory, but as a real, documented risk. The CDC and endocrine societies have warned about this for years. You deserve to know if your meds are quietly shutting down your body’s natural defenses.
Below, you’ll find real patient stories, doctor-recommended testing steps, and safe ways to manage your pain without putting your adrenal health at risk. These aren’t theoretical guides — they’re practical tools from people who’ve been there and figured out how to recover.
Opioids and Adrenal Insufficiency: A Rare but Life-Threatening Side Effect You Need to Know
Opioid-induced adrenal insufficiency is a rare but life-threatening side effect of long-term opioid use. It suppresses cortisol production and can lead to fatal adrenal crisis if undiagnosed. Learn who’s at risk and how to get tested.
