Opioid-Induced Adrenal Insufficiency Risk Assessment
This tool helps you understand your risk of opioid-induced adrenal insufficiency (OIAI) based on your medication use and symptoms. OIAI is rare but life-threatening if undiagnosed.
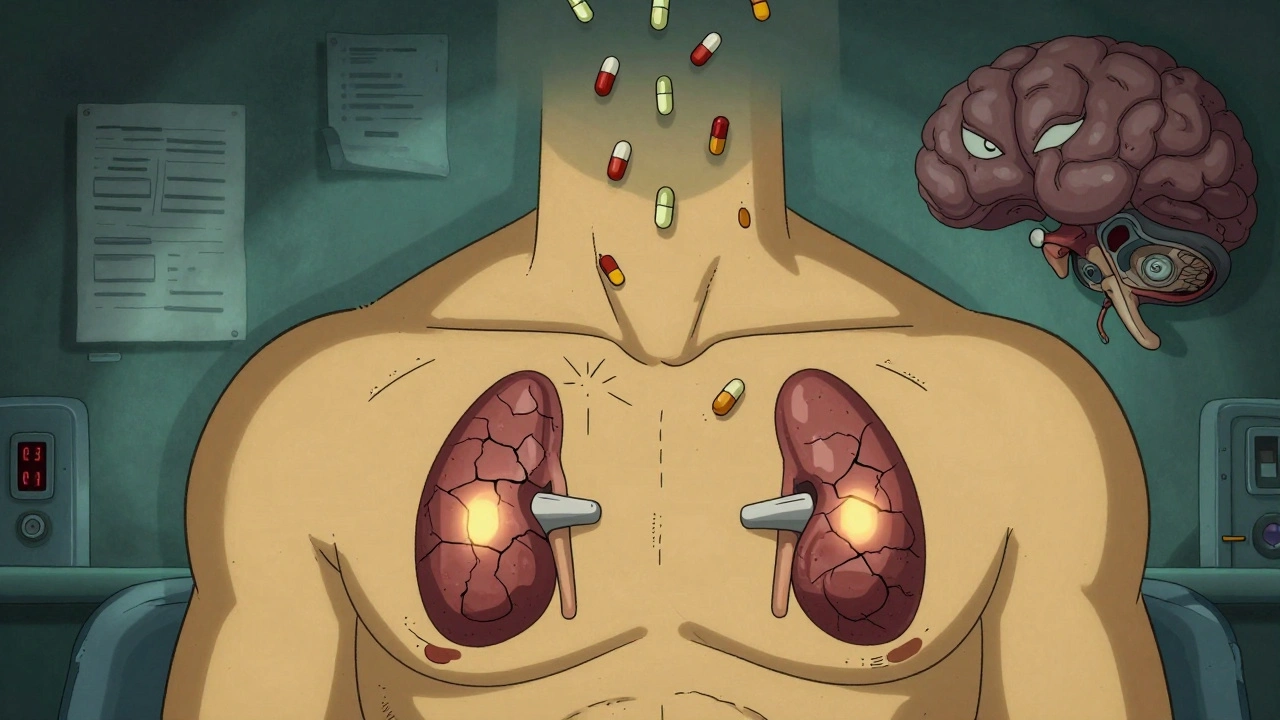
Most people know that opioids can cause constipation, drowsiness, or addiction. But few realize that long-term opioid use can quietly shut down your body’s stress response system - leading to a condition that can kill you if undiagnosed. Opioid-induced adrenal insufficiency (OIAI) is rare, but it’s not theoretical. It’s happening right now to people on chronic pain meds, and doctors are missing it.
How Opioids Silence Your Stress Hormones
Your body doesn’t make cortisol - the hormone that keeps you alive during stress - on its own. It’s a chain reaction: your brain (hypothalamus) sends a signal to your pituitary gland, which then tells your adrenal glands to release cortisol. Opioids break this chain. When you take opioids like oxycodone, hydrocodone, or methadone regularly, they bind to receptors in your brain that control this entire system. The result? Less ACTH (the signal hormone from your pituitary) and less cortisol from your adrenals. This isn’t damage to the glands themselves. It’s a silent shutdown. Your adrenals are still there, but they’re not getting the order to work. This isn’t just a lab curiosity. Studies show that about 5% of people on long-term opioid therapy develop this condition. That’s not a tiny number - it’s tens of thousands of Americans. And the risk climbs with dose. If you’re taking more than 20 morphine milligram equivalents (MME) per day, your chance of developing adrenal insufficiency jumps significantly. One study found 22.5% of long-term users failed adrenal stimulation tests, compared to 0% of people not on opioids.Why It’s So Easy to Miss
The problem isn’t that the signs are hidden - they’re just mistaken for something else. Fatigue? That’s just from chronic pain. Nausea? Side effect of the pill. Low blood pressure? Dehydration. Weight loss? Poor appetite from depression. These are all classic signs of adrenal insufficiency - but they’re also common in people with chronic illness or opioid use. So doctors don’t look for it. Even worse, some patients are already sick enough that adrenal failure gets buried under other issues. One case involved a 25-year-old man recovering from a critical illness. He developed high calcium levels - a red flag - but the real cause wasn’t cancer or parathyroid disease. It was adrenal insufficiency caused by methadone. Once he got cortisol replacement, his calcium normalized. Once he stopped the opioid, his adrenal function returned. This isn’t an outlier. Similar cases show up in people with chronic pancreatitis, back pain, or even post-surgical pain. OIAI doesn’t care if you’re on opioids for cancer or a slipped disc. If you’ve been taking them long enough and at high enough doses, your body can stop making cortisol.How Doctors Diagnose It
There’s no blood test you can take at home. Diagnosis requires a specific test: the ACTH stimulation test. Here’s how it works: your doctor draws blood to measure your morning cortisol level. If it’s below 3 mcg/dL (100 nmol/L), that’s a red flag. Then they give you a shot of synthetic ACTH and check your cortisol again after 30 or 60 minutes. If your cortisol doesn’t rise above 18 mcg/dL (500 nmol/L), your adrenal glands aren’t responding - and opioids are likely the cause. Recent research suggests even lower cortisol levels might be meaningful, especially if you’re on high-dose opioids and have symptoms. But the key isn’t just the number - it’s the context. If you’ve been on opioids for more than 90 days, especially at doses over 20 MME daily, and you’re feeling constantly tired, dizzy, or nauseous, this test should be on the table. And here’s something critical: opioids don’t affect aldosterone. That’s the hormone that controls salt and potassium. So if you have low sodium or high potassium, that’s likely not from OIAI. That points to a different problem. This distinction matters because it helps doctors rule out other causes.
What Happens If It’s Left Untreated
Adrenal insufficiency isn’t just about feeling tired. In a crisis - an infection, surgery, accident, or even severe emotional stress - your body needs cortisol to survive. Without it, you can go into an Addisonian crisis: dangerously low blood pressure, shock, vomiting, confusion, and coma. It’s fatal if not treated immediately. People with undiagnosed OIAI are walking time bombs. They might feel okay on their daily meds - until something triggers their body’s emergency response. Then, their body has no backup. Emergency rooms see these cases. Too often, the patient is misdiagnosed as having sepsis, heart failure, or a GI bug. By the time adrenal insufficiency is considered, it’s too late. That’s why experts are sounding the alarm. A 2024 review in Frontiers in Endocrinology called this an underappreciated endocrinopathy with potentially life-threatening consequences. And it’s not just a few scattered cases - it’s a pattern hiding in plain sight.Can It Be Reversed?
Yes. And that’s the good news. OIAI isn’t permanent. When opioids are tapered or stopped, the HPA axis usually wakes back up. In one case, a patient’s cortisol levels returned to normal within months after quitting methadone. Another study showed adrenal function recovered in all patients who discontinued long-term opioid therapy. But you can’t just quit cold turkey. Stopping opioids suddenly while your body still can’t make cortisol is dangerous. That’s why treatment often starts with glucocorticoid replacement - usually hydrocortisone - while the opioid dose is slowly lowered. Once the body regains its natural rhythm, the replacement can be phased out. The key is timing. If you’re on high-dose opioids and you’re scheduled for surgery, your surgeon needs to know. If you get the flu and can’t keep food down, your doctor needs to know. These are moments when your body needs extra cortisol - and if you have OIAI, you won’t make it on your own.
Who Should Be Tested
Not everyone on opioids needs a test. But if you fit any of these, ask your doctor:- You’ve been on opioids for more than 90 days
- Your daily dose is above 20 MME (morphine milligram equivalents)
- You’re constantly tired, even after sleeping
- You get dizzy when you stand up
- You’ve lost weight without trying
- You feel nauseous or have poor appetite
- You’ve had unexplained low blood pressure
The Bigger Picture
This isn’t just about one rare side effect. It’s about how we treat chronic pain. We’ve been so focused on addiction and overdose that we’ve overlooked other ways opioids can harm the body. OIAI is a reminder that opioids aren’t harmless - even when they’re prescribed legally. They change how your body works at a fundamental level. Doctors need better training. Guidelines need to update. Patients need to speak up. If you’re on long-term opioids and you’re not feeling like yourself, don’t assume it’s just the pain or the meds. Ask: Could this be my adrenal glands? Because when your body stops making cortisol, it doesn’t just make you tired. It puts your life at risk. And that’s a risk no one should take without knowing about it.Can opioid-induced adrenal insufficiency happen with short-term opioid use?
No, OIAI typically develops after prolonged use - usually more than 90 days. Short-term use, like after surgery or injury, doesn’t suppress the HPA axis enough to cause adrenal insufficiency. The condition is linked to chronic, high-dose therapy, not brief prescriptions.
Is opioid-induced adrenal insufficiency the same as Addison’s disease?
No. Addison’s disease is primary adrenal insufficiency - the adrenal glands themselves are damaged. OIAI is secondary adrenal insufficiency - the problem is in the brain’s signaling, not the glands. The treatment is similar (cortisol replacement), but the cause and reversibility are different. OIAI often reverses when opioids are stopped; Addison’s is lifelong.
Can I test for opioid-induced adrenal insufficiency at home?
No. There’s no reliable at-home test. Diagnosis requires a blood test before and after an ACTH stimulation test, which must be done in a medical setting. Symptoms alone aren’t enough - they overlap with many other conditions. Only a doctor can order and interpret the correct tests.
Does every opioid cause adrenal suppression?
Research shows that most opioids - including morphine, oxycodone, hydrocodone, methadone, and fentanyl - can suppress the HPA axis. The risk is highest with long-acting, high-dose formulations. There’s no evidence that any opioid is completely safe in this regard when used chronically at high doses.
What should I do if I’m on opioids and feel constantly exhausted?
Don’t assume it’s just the pain or the medication. Track your symptoms: fatigue, dizziness, nausea, weight loss, low blood pressure. Bring this list to your doctor and ask specifically about opioid-induced adrenal insufficiency. Request an ACTH stimulation test if you’ve been on opioids for more than 90 days and are taking more than 20 MME daily. Early detection saves lives.

Comments
Shannon Gabrielle
December 1, 2025 AT 21:30So let me get this straight-we’ve got a whole class of drugs that quietly murder your stress response and doctors are too busy checking boxes to notice? Classic American healthcare. You get addicted? That’s your fault. You stop making cortisol? That’s just bad luck.
Sean McCarthy
December 2, 2025 AT 05:26This is real. My cousin was on 80mg of oxycodone for years. He passed out in the shower. They thought it was a stroke. Turned out his cortisol was undetectable. They gave him hydrocortisone and he came back to life. No one ever tested him.
Dennis Jesuyon Balogun
December 3, 2025 AT 15:49The HPA axis is not a switch-it’s a symphony. Opioids don’t just mute one instrument; they silence the entire orchestra. We treat pain like a mechanical failure when it’s a neuroendocrine catastrophe. The reductionist model of medicine is killing people in slow motion. This isn’t side effect-it’s systemic betrayal.
And yet, we still prescribe opioids like candy because the pharmaceutical lobby owns the guidelines. The fact that 22.5% of long-term users show adrenal failure isn’t a statistical anomaly-it’s a moral indictment.
We need endocrinologists in pain clinics. We need mandatory screening. We need to stop treating chronic pain as a problem of dosage and start treating it as a problem of physiology. Your body isn’t broken-it’s been hijacked.
And the worst part? The people who need this info the most are the ones who’ve been told for years that their fatigue is ‘just in their head.’
Kshitij Shah
December 3, 2025 AT 16:41Man, I read this and thought about my uncle in Kerala. He was on tramadol for back pain for 5 years. Always tired, always dizzy. Doctors called it ‘aging.’ He died after a simple flu turned into shock. No one ever checked his cortisol. In India, this is just… invisible.
Same drugs. Same biology. Different country. Same silence.
Linda Migdal
December 4, 2025 AT 18:45Of course opioids cause adrenal suppression. The government’s been pushing them for decades to keep the working class docile. You think it’s an accident? Wake up. This is social control disguised as medicine.
They don’t want you strong. They want you numb. And now you’re too tired to protest.
Tommy Walton
December 6, 2025 AT 13:33Bro. Opioids = brain reset button. Cortisol? Gone. Like your WiFi after a router reboot. You don’t fix it by yelling at the modem. You reboot the system. Taper. Replace. Wait. Let your brain remember how to be human again. 🧠⚡
James Steele
December 7, 2025 AT 00:24Let’s not romanticize the HPA axis like it’s some sacred temple of endocrinology. It’s a feedback loop. A biological algorithm. Opioids exploit its predictability. The real tragedy isn’t the suppression-it’s the medical establishment’s refusal to acknowledge that pharmacology isn’t magic. It’s physics. And physics doesn’t care about your prescription pad.
And yet, we still treat patients like they’re broken code instead of complex systems. Pathetic.
Louise Girvan
December 7, 2025 AT 13:24They’re hiding this. They’ve always hidden this. The CDC, the AMA, Big Pharma-they knew. They knew cortisol drops. They knew people were dying in ERs with ‘sepsis’ that was really adrenal crash. But who profits when you stop prescribing opioids? Not them. So they let you die quietly.
And now you’re reading this on your phone, wondering why you can’t get out of bed. That’s not depression. That’s your adrenals screaming.
soorya Raju
December 9, 2025 AT 05:09wait so u mean to say like… opioids make ur body forget how to make cortisol?? like… its not even damage? its just… brain forgot to press the button?? this sounds like a glitch in the matrix bro. i think the gov is putting stuff in the water. also i think this is why my cousin keeps crying for no reason.
Grant Hurley
December 10, 2025 AT 22:53I’ve been on 30mg of oxycodone for 3 years. Always tired, always nauseous. Thought it was just the meds. Got tested last month. Cortisol was 1.8. They put me on hydrocortisone and I feel like I’ve been woken up from a coma. Seriously. I cried. I didn’t even know I was that tired.
Everyone on long-term opioids should get this test. No excuses. It’s free at most clinics. Just ask.
Lucinda Bresnehan
December 11, 2025 AT 14:30I’m a nurse in a pain clinic. I’ve seen this too many times. Patients come in saying ‘I just don’t have any energy’ and we chalk it up to depression or chronic pain. We never think ‘maybe their adrenals are asleep.’
I started pushing for ACTH tests for anyone on >20 MME for >90 days. We’ve caught 7 cases in 8 months. All of them improved within weeks of starting hydrocortisone. One guy went from wheelchair to walking his dog again.
It’s not complicated. It’s just overlooked. Please, if you’re on opioids and you’re tired-ask for the test. You deserve to feel alive.
ANN JACOBS
December 12, 2025 AT 02:12It is with profound concern and a deep sense of medical responsibility that I must underscore the imperative necessity of recognizing opioid-induced adrenal insufficiency as a legitimate, clinically significant, and tragically underdiagnosed endocrinological entity. The pathophysiological implications of prolonged mu-opioid receptor agonism upon the hypothalamic-pituitary-adrenal axis are not merely theoretical, but empirically validated, reproducible, and, in the context of chronic opioid therapy, alarmingly prevalent. One must consider the ethical obligation of the prescribing physician to screen for this condition, particularly in light of its potentially fatal sequelae during physiologic stress, wherein the absence of endogenous cortisol renders the patient exquisitely vulnerable to cardiovascular collapse, metabolic derangement, and death. It is therefore incumbent upon all stakeholders in healthcare-clinicians, administrators, policymakers, and patients alike-to advocate for standardized screening protocols, educational initiatives, and the integration of adrenal function assessment into routine opioid management algorithms. The lives lost to this silent epidemic are not statistics-they are individuals whose suffering was rendered invisible by institutional inertia. We must do better.
Nnaemeka Kingsley
December 12, 2025 AT 20:52Man, I been on pain meds for my back since 2020. Always felt like i was running on empty. I asked my doc about this and he looked at me like i was crazy. Then i showed him the study. He ordered the test. My cortisol was 2.1. Now i take a little hydrocortisone in the morning. I can actually play with my kids again. Dont be scared to ask. Its not weak. Its smart.