Joint Inflammation: Causes, Treatments & Practical Tips
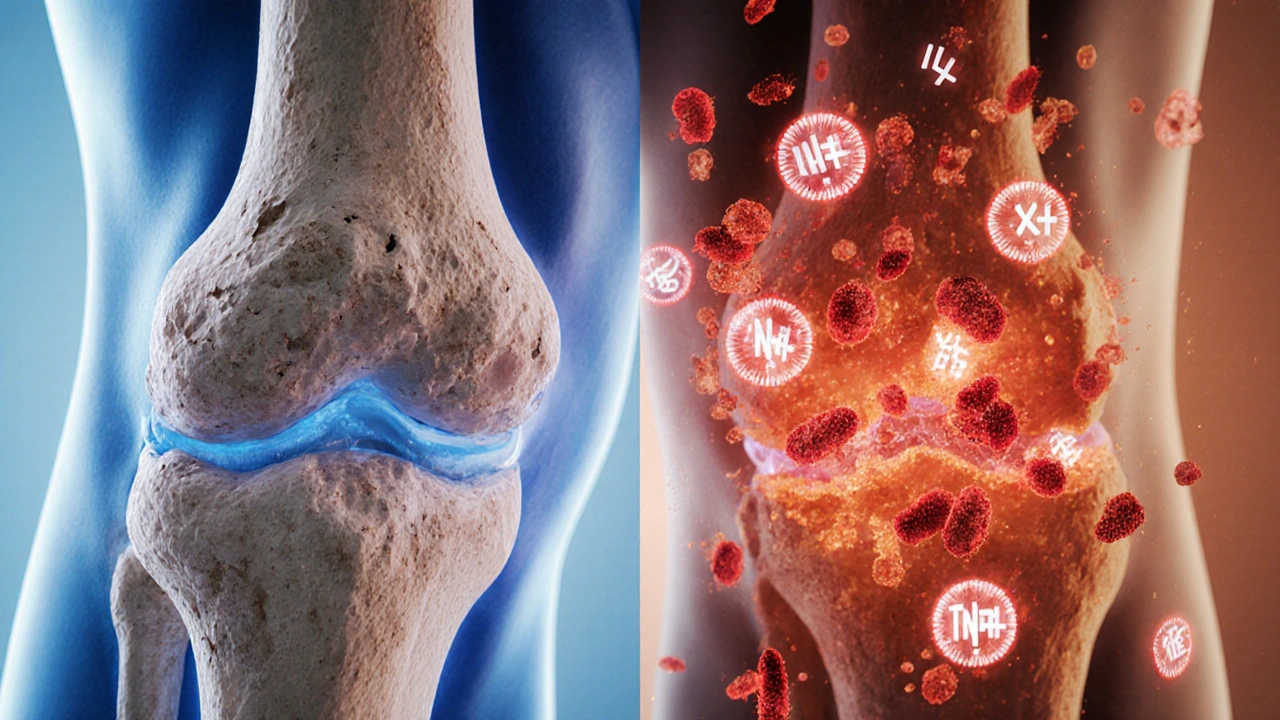
When dealing with joint inflammation, the swelling, stiffness and pain that affect a joint, often tied to arthritis, injury or infection. Also known as synovitis, it signals that your body’s immune response is targeting the joint lining. Understanding this process is the first step toward cutting the discomfort and keeping the joint moving.
One of the most common ways to calm the flare‑up is with NSAIDs, non‑steroidal anti‑inflammatory drugs such as ibuprofen, naproxen or celecoxib that block inflammatory chemicals. These meds shorten the pain cycle and lower swelling, which is why many clinicians list them as the frontline defense for joint inflammation. If NSAIDs aren’t enough, doctors may turn to corticosteroids, powerful steroids that suppress the immune system and quickly reduce severe swelling. While steroids can be very effective, they’re usually reserved for short‑term use because of possible side effects.
Beyond pills, physical therapy, targeted exercises and manual techniques that improve joint range of motion and strengthen surrounding muscles plays a huge role in long‑term control. A therapist can teach you low‑impact moves that keep the joint lubricated without overloading it, which helps prevent the next flare‑up. Pairing therapy with proper pain management, strategies like heat, cold, and mindfulness that lower the perception of pain creates a balanced approach that attacks the problem from several angles.
Key Approaches to Manage Joint Inflammation
Diet also matters. Foods rich in omega‑3 fatty acids—think salmon, walnuts, and flaxseed—have natural anti‑inflammatory properties that can complement medication. Staying hydrated supports cartilage health, and maintaining a healthy weight reduces mechanical stress on weight‑bearing joints like the knees and hips. Together, these lifestyle tweaks shrink the triggers that spark the inflammatory cascade.
Finally, monitoring is crucial. Keeping a simple log of pain levels, activity, and any new symptoms lets you and your healthcare team spot patterns early. If you notice a sudden spike in swelling, redness or fever, it could mean an infection or a more aggressive disease process that needs prompt attention. Early detection helps you adjust treatment before the joint suffers permanent damage.
Below you’ll find a curated set of articles that dive deeper into specific meds, nutrition tips, and practical steps you can take right now to tame joint inflammation and get back to moving comfortably.
How Autoimmunity Triggers Osteoarthritis: Immune System Insights
Explore how autoimmunity drives osteoarthritis, the key immune players, biomarkers, and emerging treatments that target inflammation rather than just pain.
