FDA Orphan Designation: What It Means for Rare Disease Drugs
When a drug gets FDA orphan designation, a special status given by the U.S. Food and Drug Administration to medicines targeting rare diseases affecting fewer than 200,000 people in the U.S. Also known as orphan drug status, it’s not a guarantee the drug will work—but it does unlock critical incentives to get it developed at all. Without this designation, many life-changing treatments for conditions like certain types of leukemia, rare forms of epilepsy, or inherited metabolic disorders would never make it off the lab bench.
The orphan drug, a medication specifically created to treat a rare disease or condition. doesn’t have to be brand new—it can be an old drug repurposed for a new use. That’s why you’ll see some of these drugs listed in posts about bipolar disorder, diabetes, or even skin cancer treatments. The FDA doesn’t care if the medicine treats a common condition too; what matters is whether it offers meaningful help to a small group of patients who have no other options. This is why you’ll find connections between orphan drugs and posts on medications like clobetasol for cutaneous T-cell lymphoma or nimodipine for rare neurological cases.
Behind every orphan drug is a system designed to fix a broken market. Drug companies don’t make money on treatments for diseases that affect only a few thousand people. So the FDA gives them seven years of market exclusivity, tax credits, reduced fees, and help with clinical trial design. That’s why you see so many posts here about FDA review processes, generic drug fees, and how approvals speed up—because orphan designation is one of the few levers that makes developing these drugs financially possible. It’s also why some treatments appear in lists comparing alternatives: they’re often the only option, so even if they have side effects, patients and doctors have to work with them.
Orphan designation doesn’t mean the drug is safe or better than others—it just means it’s needed. Some of these drugs come with serious risks, which is why posts about managing side effects, long-term use, or drug interactions matter so much. If you’re taking a rare disease medication, you’re not just dealing with the illness—you’re navigating a system built to support it. And that system? It’s shaped by laws like GDUFA, patient advocacy, and real-world data from people who’ve tried everything else.
Below, you’ll find real examples of how orphan-designated drugs fit into everyday treatment choices—from comparing pain relievers to understanding how long-term meds affect your body. These aren’t theoretical discussions. They’re the lived experience of patients and doctors working with limited options, trying to balance hope with safety.
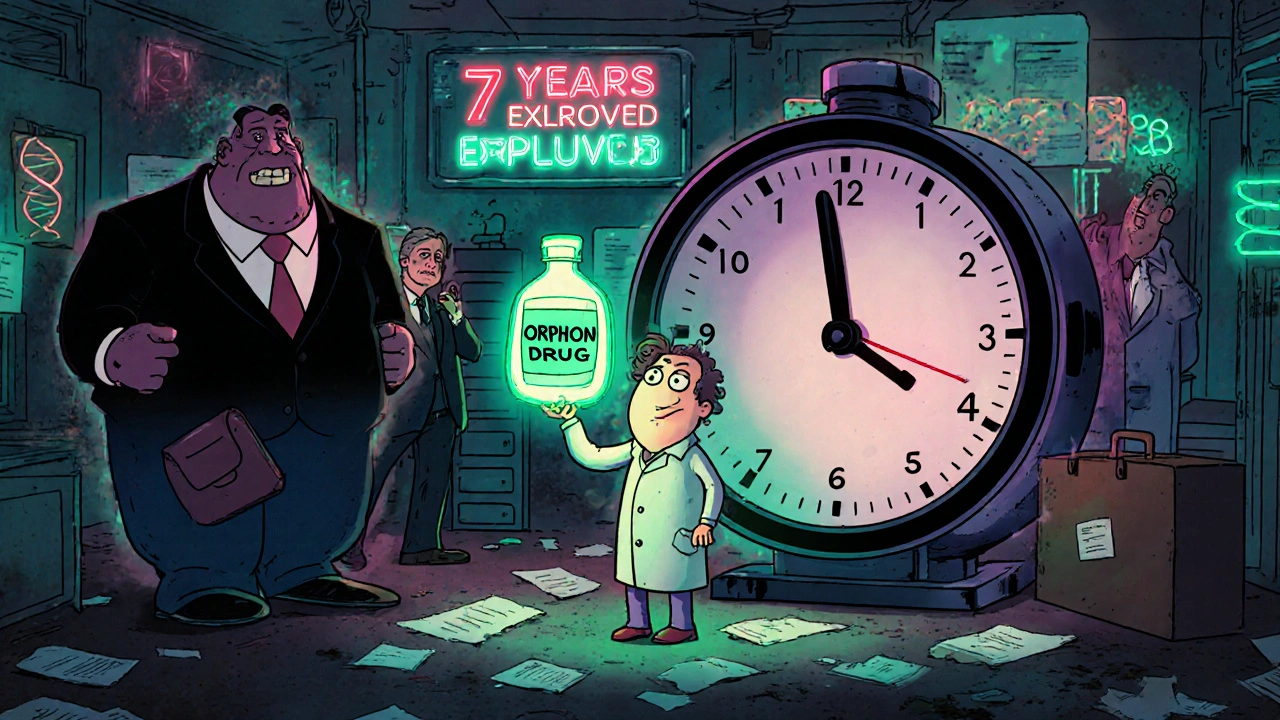
Orphan Drug Exclusivity: How Rare-Disease Medicines Get Market Protection
Orphan drug exclusivity gives pharmaceutical companies seven years of market protection for rare-disease treatments, encouraging development where profits are low. Learn how it works, why it matters, and who benefits.
