Chronic Pain Opioid Management: Safe Strategies and Real-World Choices
When dealing with long-term pain, chronic pain opioid management, the use of opioid medications to control persistent pain over months or years. Also known as long-term opioid therapy, it’s a tool that can bring relief—but only when used carefully and with clear goals. Many people start opioids for acute injuries or surgery, but when pain sticks around, the risks grow. The body adapts. Tolerance builds. Dependence can sneak in without warning. And for every person who finds real relief, another faces side effects like drowsiness, constipation, or worse—accidental overdose.
That’s why opioid safety, the set of practices designed to minimize harm while using opioid medications. Also known as responsible opioid prescribing, it isn’t just about dosage. It’s about monitoring, checking in with your doctor regularly, avoiding alcohol, and knowing the signs of trouble. It’s also about recognizing when opioids stop helping and start hurting. Studies show that after three months, opioids often lose their edge for chronic pain, while side effects pile up. That’s not failure—it’s data. And it means it’s time to rethink your plan.
What else works? pain medication alternatives, non-opioid treatments that reduce pain without the risk of addiction. Also known as multimodal pain control, it includes things like physical therapy, nerve blocks, certain antidepressants, and even cognitive behavioral therapy. These aren’t second choices—they’re often better ones. For example, duloxetine helps with nerve pain and depression at the same time. Gabapentin calms overactive nerves. Even daily walking can retrain your brain’s pain signals. And unlike opioids, none of these carry a risk of fatal overdose.
Then there’s opioid dependence, a physical state where the body needs the drug to function normally, leading to withdrawal if stopped. Also known as physical dependence, it isn’t the same as addiction, but it’s a real concern. You can be dependent on a medication without craving it or using it illegally. Still, if you’ve been on opioids for more than a few weeks, stopping cold can cause nausea, shaking, anxiety, and insomnia. That’s why tapering under medical supervision matters. No one should quit on their own.
And let’s be honest—most people don’t want to be on opioids long-term. They want to move without pain, sleep without worry, and live without fear of the next dose. That’s why pain management guidelines, evidence-based standards for treating chronic pain that prioritize safety and function over pill counts. Also known as CDC pain guidelines, it exists for a reason. They don’t say opioids are bad. They say they’re risky. And they push doctors to try everything else first.
Below, you’ll find real, practical posts that cut through the noise. You’ll see how to tell if side effects are normal or dangerous. You’ll learn how generic pain meds stack up against brand names—not in price, but in how your brain responds. You’ll find comparisons between ketorolac, ibuprofen, and other NSAIDs that might work better than opioids for your type of pain. You’ll even see how mood stabilizers and antidepressants help with nerve pain, not just depression. This isn’t theory. These are tools people use every day to get off opioids—or avoid them altogether. You don’t need to suffer. You just need the right information.
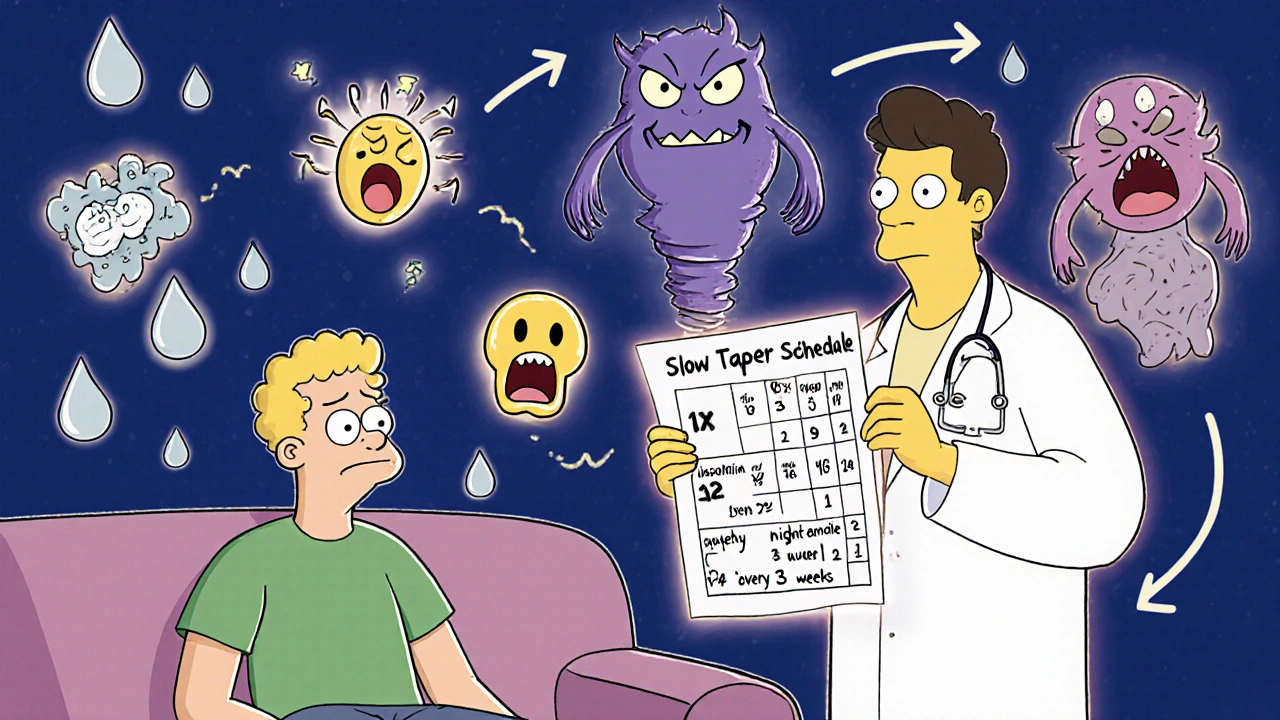
Tapering Opioids Safely: How to Reduce Side Effects and Avoid Withdrawal
Learn how to safely reduce opioid use with a slow, personalized taper to avoid severe withdrawal and dangerous side effects. Evidence-based strategies for managing pain and improving quality of life.
