Chronic Opioid Therapy: Risks, Alternatives, and Safe Management
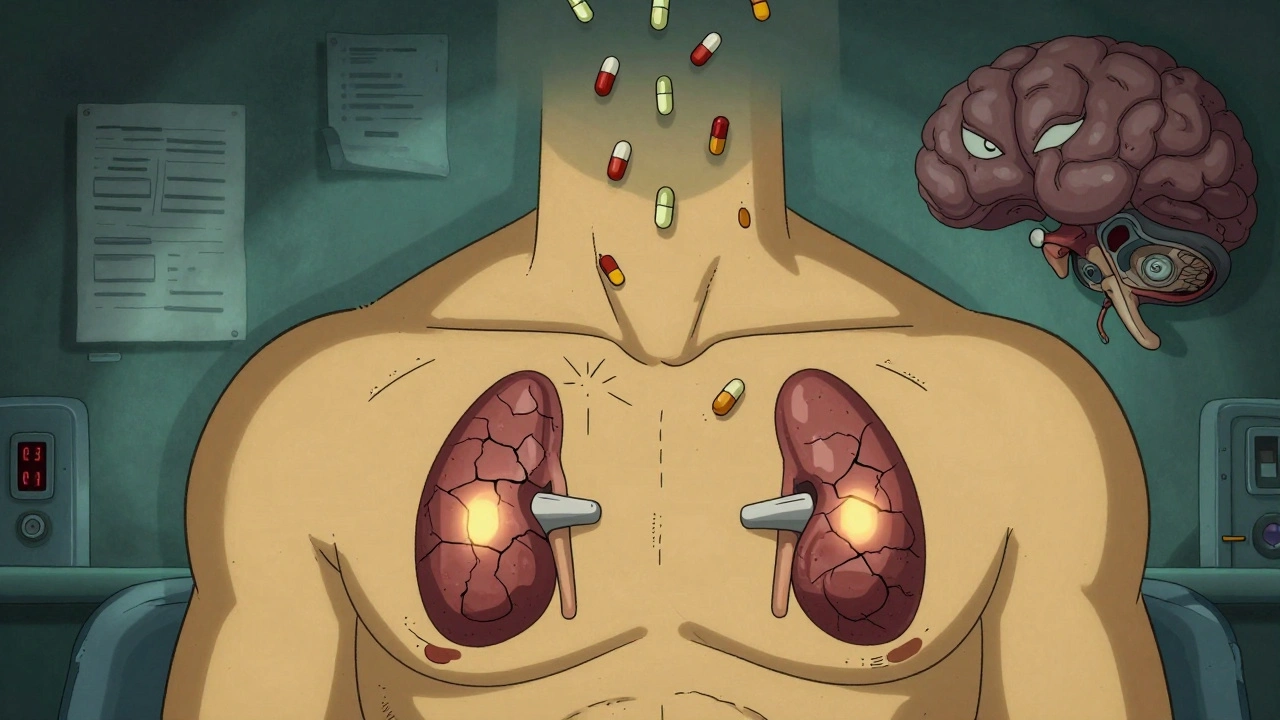
When chronic opioid therapy, the long-term use of opioid medications to manage persistent pain. Also known as long-term opioid treatment, it is often prescribed for conditions like severe arthritis, back injuries, or cancer-related pain. But it’s not a simple fix—over time, the body changes, side effects build up, and the risk of dependence grows quietly. Many people start with good intentions: relief from pain that won’t go away. But what happens after months or years? Tolerance sets in. Doses creep up. And suddenly, stopping feels impossible.
That’s where opioid tapering, a slow, controlled reduction of opioid dosage to minimize withdrawal and improve safety. Also known as opioid dose reduction, it’s not about quitting cold turkey—it’s about finding a path back to control. Studies show that people who taper slowly, under supervision, have better outcomes than those who stop abruptly. Withdrawal isn’t just nausea and sweating—it can mean insomnia, anxiety, and even depression that lasts for weeks. And if you’ve been on high doses for years, your body doesn’t bounce back overnight.
But here’s the thing: you don’t have to stay on opioids to manage pain. pain management, a broad approach that includes medication, physical therapy, psychological support, and lifestyle changes to reduce suffering. Also known as multimodal pain care, it works better than opioids alone for most long-term conditions. Think physical therapy for your back, mindfulness for your nerves, or even acupuncture for your joints. These aren’t just "alternatives"—they’re often the real solution. And when you combine them with lower-dose meds, you’re not just avoiding addiction—you’re rebuilding your life.
And if you’re already on opioids? Don’t panic. You’re not alone. Millions are in the same boat. The goal isn’t to shame or scare you—it’s to help you see your options clearly. Some people reduce their dose and feel more alert, more present, more like themselves. Others switch to non-opioid pain relievers that don’t cloud their thinking. A few find that their pain actually improves once they stop chasing the high of relief and start focusing on real healing.
The posts below cover exactly this: how to recognize when opioids are doing more harm than good, how to talk to your doctor about cutting back, what side effects to watch for, and what actually works when opioids aren’t the answer anymore. You’ll find real stories, practical steps, and clear comparisons—no fluff, no jargon, just what you need to make smarter choices for your body and your future.
Opioids and Adrenal Insufficiency: A Rare but Life-Threatening Side Effect You Need to Know
Opioid-induced adrenal insufficiency is a rare but life-threatening side effect of long-term opioid use. It suppresses cortisol production and can lead to fatal adrenal crisis if undiagnosed. Learn who’s at risk and how to get tested.
