Biomarkers – What They Are and Why They Matter
When working with biomarkers, biological indicators that signal normal or abnormal processes, conditions, or responses to therapy. Also known as biological markers, they help doctors and researchers detect disease early, track treatment, and predict outcomes. In everyday language, think of a biomarker as the body’s own traffic sign – it tells you when everything’s running smoothly or when something’s going off‑track.
One of the biggest ways biomarkers show up is in diagnostic tests, procedures that measure specific markers to confirm or rule out a condition. Whether it’s a blood glucose reading for diabetes or a PSA level for prostate health, these tests rely on biomarkers to turn invisible chemistry into clear numbers you can act on. Biomarkers are the backbone of personalized medicine, an approach that tailors treatment to an individual’s unique biological profile. By matching the right drug to the right marker, doctors can boost effectiveness and cut side effects.
Beyond diagnosis and treatment matching, biomarkers drive risk assessment, the process of estimating a person’s likelihood of developing a disease based on measurable indicators. Elevated cholesterol particles, specific genetic variants, or inflammatory proteins all feed into a risk score that guides lifestyle changes or preventive medication. In the research arena, clinical trials, studies that test new therapies in humans, depend on biomarkers to gauge whether a drug hits its target, how patients respond, and when to stop or adjust the study.
How Biomarkers Shape Modern Healthcare
Biomarkers encompass disease detection, treatment monitoring, and outcome prediction – a triple role that makes them indispensable. Personalized medicine requires reliable biomarkers to choose the right therapy, while diagnostic tests rely on biomarkers to deliver accurate results. Risk assessment is guided by biomarker levels, and clinical trials use biomarkers to measure drug efficacy. This network of relationships means that a single marker can influence everything from a routine lab order to a multi‑year drug development program.
Take cancer, for example. The HER2 protein acts as a biomarker that tells oncologists whether a patient will benefit from trastuzumab. In heart disease, troponin levels signal heart muscle injury, prompting emergency care and informing long‑term medication plans. Even mental health is catching up – certain inflammatory markers are being studied as biomarkers for depression treatment response. These real‑world cases illustrate how biomarkers turn complex biology into actionable information.
For patients, understanding your own biomarkers can empower better conversations with your healthcare team. Asking about what your latest lab results mean, whether they indicate a heightened risk, or how they influence the next step in your care plan puts you in the driver’s seat. For clinicians, staying current on emerging biomarkers means faster adoption of cutting‑edge therapies and more precise patient stratification.
Below you’ll find a curated collection of articles that dig deeper into specific biomarkers, explain how to interpret test results, and offer practical tips for using this information in everyday health decisions.
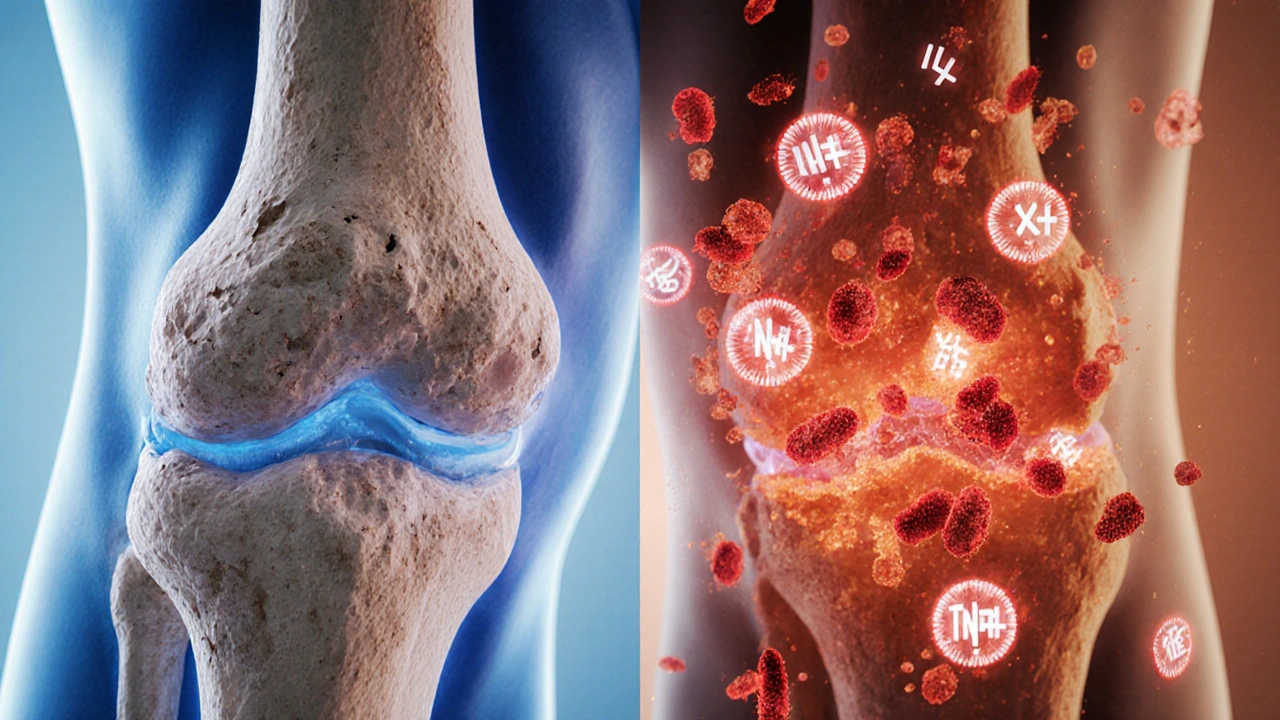
How Autoimmunity Triggers Osteoarthritis: Immune System Insights
Explore how autoimmunity drives osteoarthritis, the key immune players, biomarkers, and emerging treatments that target inflammation rather than just pain.
