Vitamin D & Calcium Level Checker
About Vitamin D & Calcium
Vitamin D plays a crucial role in calcium absorption and maintaining healthy blood calcium levels. Low vitamin D can lead to hypocalcemia, causing muscle cramps, tingling, and other symptoms.
For best results, ensure your vitamin D level is above 30 ng/mL and calcium is within normal range (8.5–10.5 mg/dL).
Vitamin D is more than just a sunshine vitamin - it’s the linchpin that keeps our calcium levels steady and our bones strong. If you’ve ever wondered why a simple nutrient can stop a drop in blood calcium, read on.
Key Takeaways
- Hypocalcemia occurs when blood calcium falls below 8.5mg/dL and can cause muscle cramps, tingling, or even cardiac issues.
- Vitamin D boosts calcium absorption from the gut and works with parathyroid hormone to keep calcium in the bloodstream.
- Most adults need 600-800IU of vitamin D daily; higher doses may be needed for people with limited sun exposure.
- Safe sources include fortified dairy, fatty fish, eggs, and regular outdoor time; supplements fill the gap when diet or sunlight fall short.
- Monitoring serum 25(OH)D levels and calcium tests helps catch deficiencies before symptoms appear.
What Is Hypocalcemia?
Hypocalcemia is a medical term for low calcium in the blood. Normal serum calcium ranges from 8.5 to 10.5mg/dL. When it dips below that window, nerve and muscle cells become hyper‑excitable, leading to tingling (paresthesia), muscle twitching, and in severe cases, seizures or abnormal heart rhythms.
Causes range from vitamin D deficiency and low dietary calcium to surgical removal of the parathyroid glands, kidney disease, or certain medications. Understanding the role of vitamin D helps address the most common-and preventable-cause.
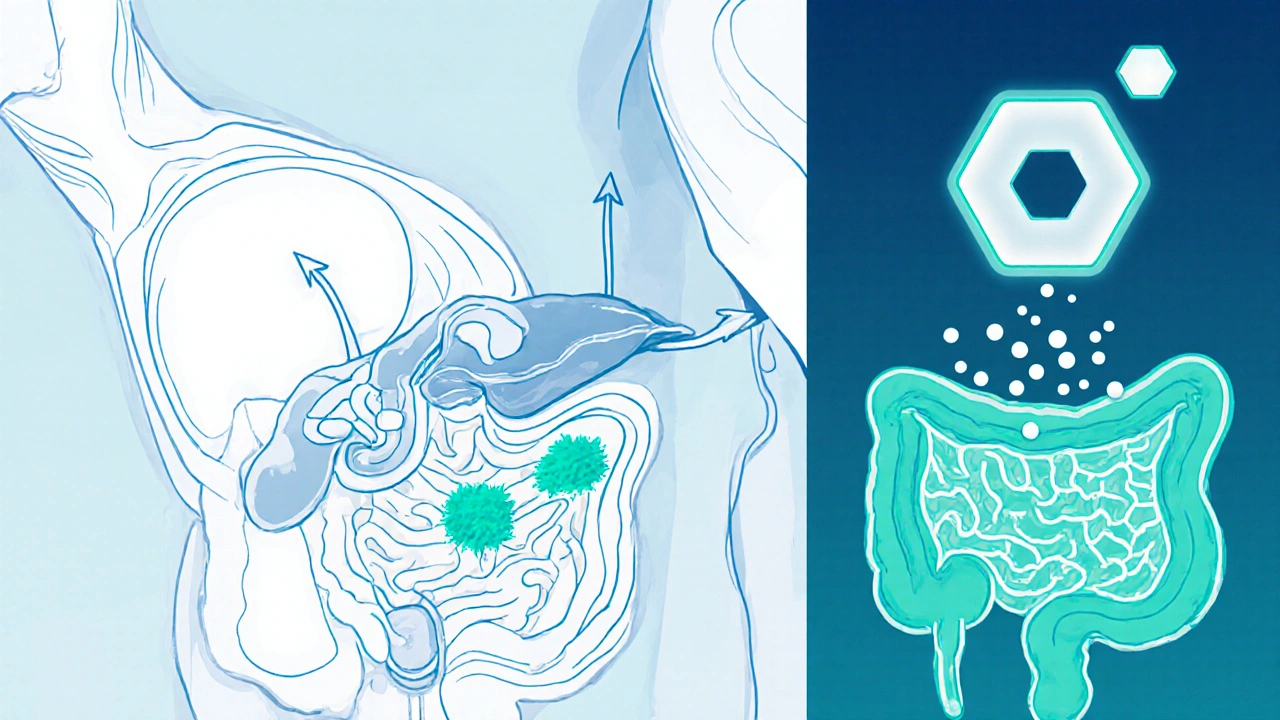
How Vitamin D Keeps Calcium in Check
Vitamin D is a fat‑soluble vitamin that functions like a hormone. Once activated to calcitriol (1,25‑dihydroxyvitaminD), it binds to receptors in the intestinal lining, boosting the expression of calcium‑transport proteins. This process lifts calcium absorption from roughly 10% to 30‑40% of what you eat.
The same active form also talks to the parathyroid hormone (PTH). When blood calcium falls, PTH spikes, prompting the kidneys to convert more vitamin D to its active form, releasing calcium from bones, and reducing calcium loss in urine. In short, vitamin D and PTH form a feedback loop that stabilizes calcium levels.
If vitamin D levels are insufficient, the gut can’t pull enough calcium, and the feedback loop falters. The body then leans heavily on bone resorption, weakening the skeleton and still failing to normalize blood calcium - a recipe for hypocalcemia.
Recommended Vitamin D Intake and Sources
The Institute of Medicine sets the Recommended Dietary Allowance (RDA) at 600IU (15µg) for adults up to age 70, and 800IU (20µg) for older adults. In Australia, the National Health and Medical Research Council backs similar numbers, noting that people with darker skin, limited sun, or indoor lifestyles may need up to 2,000IU daily.
Here’s a quick look at the most reliable sources:
| Source | Typical IU (International Units) | Pros | Cons |
|---|---|---|---|
| Sunlight (10‑15min, mid‑day, face & arms) | ~1,000‑5,000 | Free, natural production | UV risk, variable by season & latitude |
| Fortified skim milk (1cup) | ~120 | Widely available, adds calcium | Lactose intolerance for some |
| Salmon (cooked, 100g) | ~570 | High omega‑3, protein | Cost, mercury concerns for certain species |
| Egg yolk (1 large) | ~40 | Easy to incorporate | Low IU per serving |
| Vitamin D3 supplement (500IU tablet) | 500 (as labeled) | Precise dosing, works year‑round | Risk of overdose if combined with fortified foods |
For most Australians, a mix of outdoor activity and fortified foods covers the RDA. If you live in Perth’s sunny climate, 10‑15minutes of midday sun a few times a week often suffices. However, during winter or for those who spend most time indoors, a supplement becomes essential.

Who Is at Risk of Vitamin D Deficiency?
Even in sunny regions, certain groups struggle to maintain adequate levels:
- Older adults - skin loses the ability to synthesize vitamin D efficiently.
- People with darker skin - melanin blocks UV‑B rays.
- Those who wear covering clothing for cultural or occupational reasons.
- Individuals with malabsorption syndromes (celiac disease, Crohn’s disease) - vitamin D is fat‑soluble and needs healthy gut lining.
- Patients on certain meds like anticonvulsants or glucocorticoids, which accelerate vitamin D breakdown.
Screening involves measuring serum 25‑hydroxyvitamin D (25(OH)D). Levels below 20ng/mL (50nmol/L) denote deficiency, 20‑30ng/mL is insufficient, and 30‑50ng/mL is considered adequate for bone health.
Practical Steps to Prevent Hypocalcemia
- Assess your sun exposure. Aim for 10‑15minutes of midday sun on face, arms, and legs, 2‑3 times weekly during the warmer months.
- Include vitamin D‑rich foods in daily meals. A breakfast of fortified cereal with milk and a boiled egg adds roughly 160IU.
- Consider a supplement if you fall into a high‑risk category. A 1,000IU vitamin D3 tablet taken with a fatty meal ensures optimal absorption.
- Check your calcium intake. Adults need about 1,000mg per day (1,200mg for women over 50). Dairy, leafy greens, tofu, and fortified plant milks help meet the target.
- Schedule a blood test every 1‑2years, especially if you’re over 60, have limited sun, or take meds that affect vitamin D metabolism.
- If your serum calcium is low, your doctor may order a quick serum calcium test, followed by vitamin D level assessment, to pinpoint the cause.
- Follow medical advice on calcium supplementation only when prescribed. Excess calcium without adequate vitamin D can lead to kidney stones.
Sticking to these habits keeps the calcium‑vitaminD partnership running smoothly, reducing the chance of hypocalcemia and its uncomfortable symptoms.
Frequently Asked Questions
Can I get enough vitamin D from food alone?
Most people need a combination of diet and sunlight. Fatty fish, fortified dairy, and egg yolks provide modest IU amounts, but meeting the full RDA without sunlight often requires a supplement, especially in winter or for high‑risk groups.
What symptoms signal low calcium?
Early signs include tingling around the mouth and fingers, muscle cramps, and fatigue. Severe hypocalcemia can cause seizures, spasms (tetany), and irregular heartbeats.
Is it safe to take high‑dose vitamin D pills?
Short‑term high doses (e.g., 50,000IU weekly) are sometimes prescribed to correct deficiency, but chronic excess can cause hypercalcemia. Always follow a doctor’s guidance and avoid stacking multiple fortified products.
How often should I test my vitamin D levels?
For healthy adults with regular sun exposure, testing every 2‑3years is enough. High‑risk individuals should test annually or after any change in medication or lifestyle that affects vitamin D metabolism.
Can sunscreen block vitamin D production?
Sunscreen with SPF30 can reduce UV‑B exposure by about 95%, potentially limiting vitamin D synthesis. A brief, uncovered exposure before applying sunscreen balances skin protection with vitamin D needs.


Comments
Dipankar Kumar Mitra
October 7, 2025 AT 13:44Ever feel like the sun is whispering secrets to your bones? Vitamin D is that elusive whisper, pulling calcium from the gut like a magnetic tide. When the levels dip below the magic 30 ng/mL, your blood calcium starts to wobble, and the whole system feels the ache. Think of it as the body’s silent alarm that you’ve ignored the light.
Tracy Daniels
October 17, 2025 AT 21:14Vitamin D isn’t just another nutrient; it’s a critical co‑factor that facilitates intestinal calcium absorption, ensuring serum calcium remains within the narrow 8.5–10.5 mg/dL window. Maintaining serum 25(OH)D above 30 ng/mL dramatically reduces the risk of hypocalcemia‑related symptoms such as muscle cramps and paresthesia. For most individuals, 15–20 minutes of midday sunlight a few times a week suffices, but dietary supplementation can bridge gaps when exposure is limited. Remember to have your levels checked annually, especially if you have risk factors like limited sun exposure, darker skin, or malabsorption syndromes. 😊
Hoyt Dawes
October 28, 2025 AT 03:44Honestly, the whole “check your levels” gimmick feels like a repackaged wellness fad aimed at the easily swayed. If you’re already reading about serum 25‑hydroxyvitamin D, you’re probably too deep into the rabbit hole to care about milk‑drunk trends. Still, the science does have a kernel of truth buried beneath the hype.
Jeff Ceo
November 7, 2025 AT 11:14Let’s cut the theatrics-low vitamin D directly impairs active calcium transport in the enterocytes, which is why hypocalcemia can manifest so quickly when deficiency persists. It’s not a mere buzzword; it’s a physiological bottleneck.
David Bui
November 17, 2025 AT 18:44Look mate the body doesn’t care about your trend‑setting diet if the sun ain’t doing its job – you’ll still end up with shaky calcium numbers. Even a bit of outdoor time beats a dozen fancy supplements, honestly.
Alex V
November 28, 2025 AT 02:14Oh, sure, just pop a bottle of “sunshine in a capsule” and expect your bones to start doing the tango. As if the endocrine orchestra ever takes a coffee break because you missed a morning jog. The reality? Vitamin D receptors need to be saturated before calcium even gets a foot in the door, and most of us are stuck at the lobby.
Robert Jackson
December 8, 2025 AT 09:44Brits have always known the power of a good walk in the rain, yet we ignore the simple fact that sunlight is a right, not a luxury.
Maricia Harris
December 18, 2025 AT 17:14Can we just acknowledge how dramatic it is when someone blames “low calcium” on just “not enough sun”? The body’s a drama queen itself.
Tara Timlin
December 29, 2025 AT 00:44Great tool for tracking vitamin D and calcium levels!
Jean-Sébastien Dufresne
January 8, 2026 AT 08:14Indeed, the correlation between serum 25‑hydroxyvitamin D and calcium homeostasis is not merely coincidental, it is a cornerstone of skeletal health, especially in regions where sunlight is scarce, and supplementation becomes indispensable, therefore regular monitoring is advisable. 😊
Patrick Nguyen
January 18, 2026 AT 15:44Serum 25‑hydroxyvitamin D levels below 30 ng/mL impede active calcium absorption, leading to potential hypocalcemia. Routine assessment is advisable for at‑risk populations.
Patrick Bread
January 28, 2026 AT 23:14It is fascinating how often the simplest biochemical pathways are obscured by hype. One would think that the medical community would simply advise sunlight exposure, yet we get endless supplement podcasts. Nonetheless, the mechanistic link remains unequivocal.
Fiona Doherty
February 8, 2026 AT 06:44Enough with the sugar‑coated health advice – if your D level is low, your calcium will suffer, period. Get tested and fix it.
Neil Greer
February 18, 2026 AT 14:14First, let’s acknowledge that vitamin D’s role in calcium metabolism is a textbook example of a co‑factor enabling a critical physiological process; without sufficient 25‑hydroxyvitamin D, the intestinal epithelial cells cannot efficiently up‑regulate the calcium‑binding proteins required for active transport. Second, the feedback loop involving parathyroid hormone (PTH) becomes hyperactive when serum calcium dips, which, over time, can lead to secondary hyperparathyroidism and bone demineralization. Third, epidemiological studies consistently show that populations with lower sun exposure have higher incidences of hypocalcemia‑related complications, reinforcing the biochemical data. Fourth, the threshold of 30 ng/mL for vitamin D sufficiency is not arbitrary; it reflects the point at which the maximum expression of calbindin is achieved. Fifth, patients with malabsorption syndromes, such as celiac disease, often require both higher vitamin D intake and calcium supplementation to overcome the dual barrier. Sixth, the interaction with magnesium is also crucial, as magnesium deficiency can blunt the activation of vitamin D, creating a vicious cycle. Seventh, genetic polymorphisms in the vitamin D receptor can modulate individual responses, meaning some people may need higher serum levels to achieve the same calcium absorption efficiency. Eighth, the seasonal variation in vitamin D synthesis explains why winter months see a spike in hypocalcemic symptoms in temperate regions. Ninth, dietary sources like fortified dairy provide a reliable, albeit modest, contribution to overall vitamin D status, but they rarely replace sun exposure. Tenth, supplementation strategies should be tailored-daily low‑dose regimens versus intermittent high‑dose loading-based on baseline serum levels and patient compliance. Eleventh, clinicians should interpret calcium labs in the context of albumin levels, as total calcium can be misleading without correction. Twelfth, ionized calcium measurement offers a more accurate snapshot of physiologically active calcium, especially in critical care settings. Thirteenth, patient education is vital; many individuals are unaware that over‑the‑counter vitamin D supplements can vary widely in potency. Fourteenth, public health policies encouraging safe sun exposure and fortified foods can mitigate widespread deficiencies. Finally, regular monitoring, combined with individualized supplementation, ensures that both vitamin D and calcium remain in harmony, preventing the cascade of metabolic disturbances that can culminate in fractures, muscle weakness, and cardiovascular complications.
Fionnuala O'Connor
February 28, 2026 AT 21:44Stay consistent with your testing and you’ll see progress – keep it simple