Left ventricular dysfunction: what it means and what you can do
Left ventricular dysfunction means the heart’s main pumping chamber (the left ventricle) isn’t working as well as it should. That can make you feel tired, short of breath, or swollen in the legs. Some people have mild changes and no symptoms; others develop heart failure. Knowing the signs, tests, and everyday steps helps you stay ahead of problems.
What is left ventricular dysfunction?
There are two main types. Systolic dysfunction (HFrEF) happens when the ventricle can’t squeeze strongly, so less blood goes out to the body. Diastolic dysfunction (HFpEF) means the ventricle is stiff and can’t fill properly. Both reduce the heart’s ability to supply organs and muscles with oxygen-rich blood.
Common causes include coronary artery disease (blocked arteries), high blood pressure, heart attacks, valve problems, long-term alcohol use, infections, and some medicines or toxins. Age and chronic conditions like diabetes also raise the risk.
Diagnosis and treatment — what to expect
If a doctor suspects left ventricular dysfunction, they’ll ask about symptoms and do a physical exam. Typical tests: an ECG (heart rhythm), blood tests including BNP/NT-proBNP (markers of stress on the heart), chest X-ray, and an echocardiogram (ultrasound) that shows how well the left ventricle pumps. Sometimes a stress test, coronary angiogram, CT or MRI are needed.
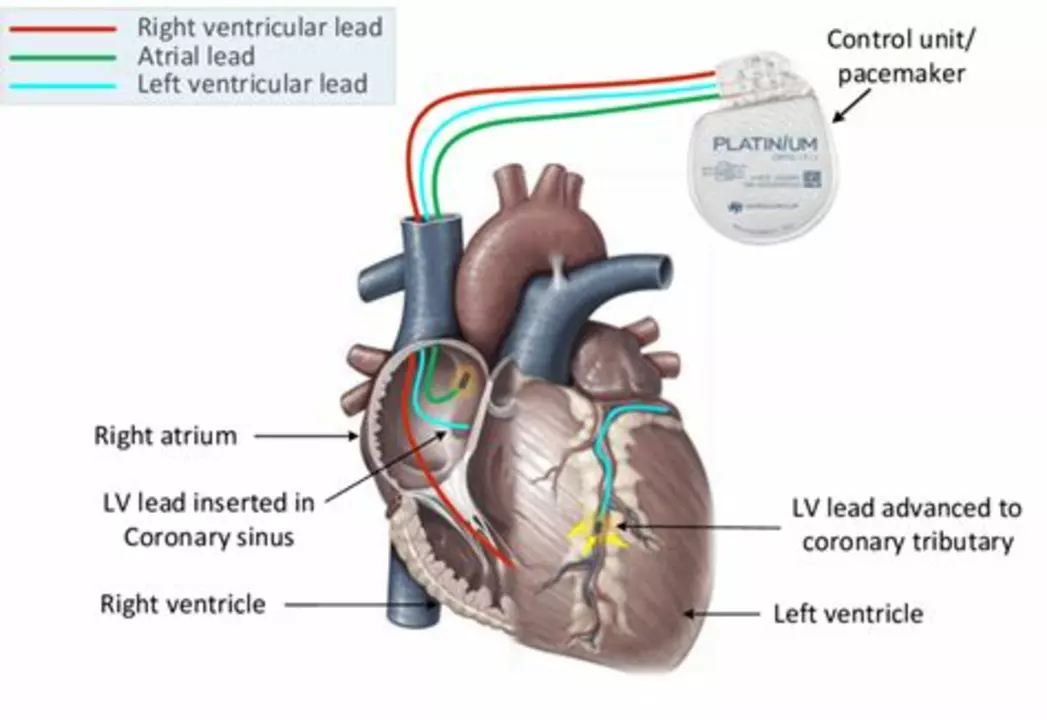
Treatment aims to reduce symptoms, prevent worsening, and lower the risk of hospital visits and death. Common medicines include ACE inhibitors or ARBs, beta blockers, mineralocorticoid receptor antagonists, and newer drugs like ARNI and SGLT2 inhibitors. Diuretics help control fluid build-up. In some cases, devices such as a pacemaker with cardiac resynchronization (CRT) or an implantable defibrillator (ICD) are recommended. Valve repair, bypass surgery, or advanced therapies may be needed for specific problems.
Lifestyle changes matter. Cut back on sodium, track your weight daily, limit alcohol, stay active within your limits, and stop smoking. Vaccines (flu and pneumococcal) can prevent infections that stress the heart. Follow-up care and medicine adjustments are normal — this is a long-term condition for many people.
Watch for red flags: sudden weight gain (2–3 kg in a few days), worsening shortness of breath at rest or while lying flat, fainting, or swelling that gets worse quickly. These need urgent medical attention.
Living with left ventricular dysfunction means working with your care team. Ask about goals for your medicines, how often to check blood tests, and when to call for help. Small daily habits—tracking symptoms, taking meds on time, and staying active—often make a big difference.
The Importance of Patient Education in Managing Left Ventricular Dysfunction
As a blogger, I cannot emphasize enough the importance of patient education in managing left ventricular dysfunction. Educating patients helps them understand their condition better and empowers them to take an active role in managing their health. It's crucial for patients to know how to recognize symptoms and when to seek medical help. Furthermore, understanding the benefits of prescribed medications and lifestyle changes can significantly improve adherence to treatment plans. Ultimately, informed patients are more likely to achieve better health outcomes, reducing the burden on healthcare systems.
