Statin Intolerance Assessment Tool
Many people experience muscle pain after starting statins, but not all of these symptoms are actually caused by the medication. This tool will help you understand if your symptoms may be related to statin intolerance or if other factors might be the cause.
What Is Statin Intolerance, Really?
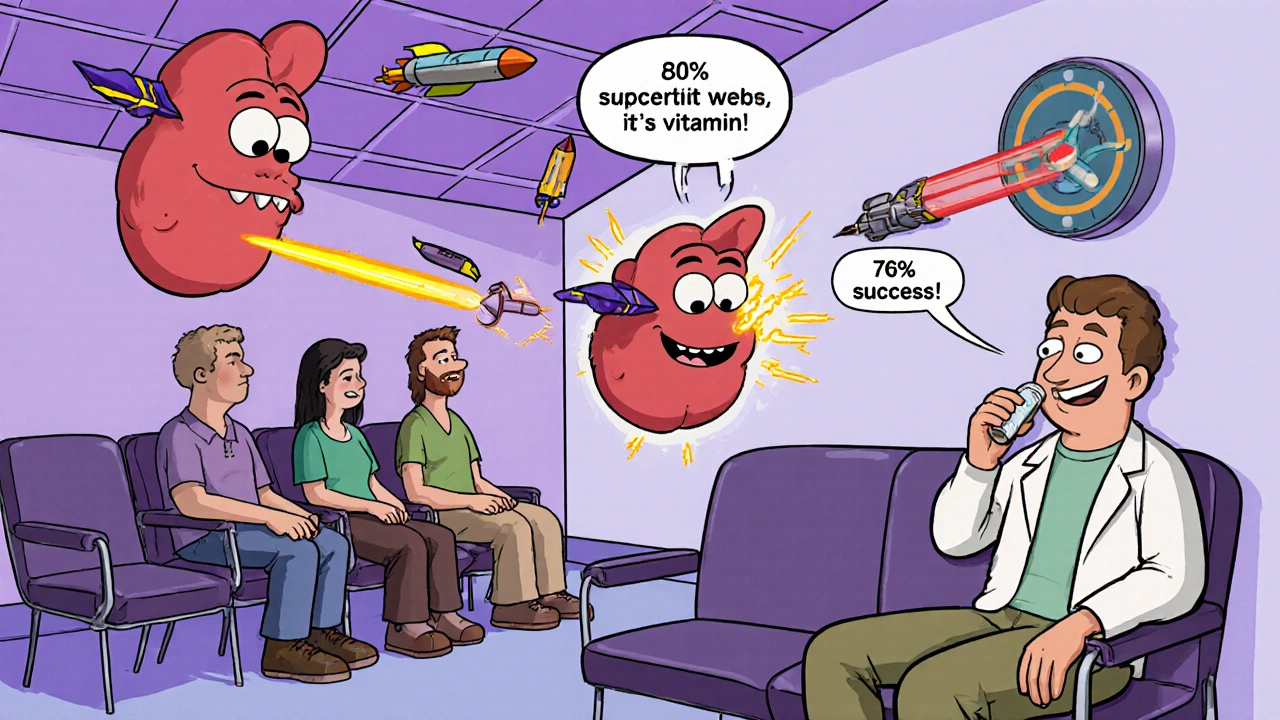
Many people hear they’re "statin intolerant" and assume they can never take cholesterol-lowering medication again. But that’s often not true. Statin intolerance isn’t a one-size-fits-all diagnosis-it’s a process. It means you’ve had side effects, usually muscle pain or weakness, that made you stop taking a statin. But here’s the catch: statin intolerance is frequently misdiagnosed. Studies show up to 80% of people who think they can’t tolerate statins actually can, once they’re tested properly.
The real problem? Most patients are told to stop statins after one bad reaction, without a clear plan to figure out why. That’s where specialized clinics come in. These aren’t flashy new hospitals-they’re often just lipid specialists and pharmacists working within existing cardiology departments, using proven, step-by-step protocols to get patients back on effective treatment.
How Do You Know It’s Really the Statin?
Not every muscle ache is caused by statins. Other things can mimic statin side effects: low thyroid function, vitamin D deficiency, overtraining, or even other medications like antibiotics or fibrates. A proper statin intolerance clinic doesn’t just stop the drug-they investigate everything else first.
The standard approach? Stop the statin for two full weeks. If your symptoms fade during that time, it’s a strong clue the statin was the culprit. Then, under medical supervision, you rechallenge with a different statin-usually a hydrophilic one like rosuvastatin or pravastatin. These are less likely to leak into muscle tissue because they’re designed to be taken up by the liver, not the muscles.
Some clinics also check your creatine kinase (CK) levels. If your CK is more than 10 times the normal upper limit, that’s a red flag. But here’s the key: many patients have muscle pain with normal CK. That’s why diagnosis now focuses more on symptoms and timing than blood tests alone. The pattern? Pain starts 2-4 weeks after starting the statin and goes away 2-4 weeks after stopping it. That’s the hallmark of true statin-associated muscle symptoms (SAMS).
The Four-Step Protocol That Works
Leading clinics like Cleveland Clinic and Kaiser Permanente follow a clear, evidence-based path. It’s not guesswork-it’s a checklist.
- Stop the statin. Discontinue all statins for at least 14 days. Keep a symptom diary: rate pain on a scale of 0-10, note which muscles hurt, and track when it started and stopped.
- Rule out other causes. Test thyroid function, vitamin D, and check for drug interactions. Alcohol, certain supplements, and even intense exercise can make muscle symptoms worse.
- Rechallenge with a different statin. Try a hydrophilic statin (rosuvastatin or pravastatin) at the lowest dose. If that fails, try a lipophilic statin with a different metabolic pathway, like fluvastatin.
- Try intermittent dosing. If daily dosing still causes issues, switch to every-other-day or twice-weekly dosing. Rosuvastatin, with its long half-life, works well for this. Studies show 76% of previously intolerant patients tolerate this approach and still lower LDL by 20-40%.
This isn’t just theory. At the VA system, which rolled this out across 170 centers, false diagnoses dropped by 38%. That means thousands of people who were told they couldn’t take statins were given a second chance-and many got their cholesterol under control without pain.

What If You Still Can’t Tolerate Any Statin?
For the 5-15% who truly can’t take any statin-even at low or intermittent doses-there are other options. The first-line alternative is ezetimibe. It’s cheap ($35 a month), safe, and proven in the IMPROVE-IT trial to reduce heart attacks and strokes by 6%. It works by blocking cholesterol absorption in the gut.
If that’s not enough, bempedoic acid (Nexletol) is a newer option. Approved in 2020, it lowers LDL by about 18% and doesn’t cause muscle side effects because it’s activated only in the liver, not in muscle tissue. It costs more-around $491 a month-but it’s a game-changer for patients who’ve exhausted other options.
PCSK9 inhibitors like evolocumab are even more powerful, lowering LDL by 50-60%. But they’re expensive-about $5,850 a year-and insurance often denies them unless you’ve tried and failed everything else. Many patients spend months appealing these decisions.
What’s important to know: none of these alternatives match the full cardiovascular benefit of statins. Statins reduce major heart events by 20-25% for every 1 mmol/L drop in LDL. Ezetimibe gives about half that. PCSK9 inhibitors are close, but only if you can get them.
Real Patient Stories: What Works and What Doesn’t
One patient, who posted on Reddit under "HeartPatient87," had been told he was statin intolerant for five years. He was on no cholesterol meds, and his LDL was 142. After visiting a lipid clinic at Johns Hopkins, he was switched to rosuvastatin 5 mg twice a week, plus CoQ10. His LDL dropped to 89. No muscle pain. He’s been on it for two years.
Another patient on the Inspire forum spent 11 weeks fighting insurance to get access to a PCSK9 inhibitor. She met all clinical criteria, but her plan required four appeals. She eventually got it-but only after her doctor wrote a letter explaining her high heart disease risk.
Meanwhile, Kaiser Permanente’s internal data shows 82% of patients in their statin intolerance program were able to restart lipid-lowering therapy. In regular clinics, only 45% could. The difference? Structure. A clear plan. Follow-up. And a team that doesn’t give up.
Why Most Doctors Don’t Do This
It’s not that doctors don’t care. It’s that they’re overwhelmed. Most primary care doctors don’t have time to run a two-week rechallenge, order multiple tests, and manage complex alternatives. Statin intolerance clinics work because they’re designed for this one thing: managing patients who failed statins.
These clinics often include pharmacists who specialize in lipid therapy. At Cleveland Clinic, pharmacists lead the rechallenge process-and their success rate is 22% higher than when doctors do it alone. That’s because pharmacists track dosing schedules, drug interactions, and side effects with precision.
Also, many doctors still believe statin side effects are mostly psychological. And yes, the nocebo effect is real. If you’ve been told statins cause muscle pain, you’re more likely to feel it-even if the pill is a placebo. That’s why blinded rechallenges (where you don’t know if you’re getting the real drug) are the gold standard. But they’re hard to do in regular practice.
What’s Coming Next
Genetic testing is starting to play a role. Some people have a variant in the SLCO1B1 gene that makes them more likely to get muscle pain from simvastatin. Mayo Clinic began testing for this in 2023. If you carry the variant, you avoid simvastatin altogether.
There’s also new tech on the horizon: nanoparticle-delivered statins. These tiny particles target the liver directly, bypassing muscle tissue. Early trials show 92% tolerability. They’re still in phase 2, but if they work, they could change everything.
And intermittent dosing? It’s gaining serious traction. In 2024, 78% of lipid specialists said they plan to use it more. It’s cheap, safe, and effective for many who can’t take daily pills.
How to Find a Statin Intolerance Clinic
These clinics aren’t everywhere. They’re mostly in academic medical centers or large health systems. If you’re struggling with statin side effects, ask your doctor for a referral to a lipid specialist. Look for clinics affiliated with universities or hospitals that have cardiology departments.
Some resources can help:
- The National Lipid Association’s Statin Intolerance Management Toolkit (updated quarterly, used by over 12,000 clinicians in 2024)
- The American College of Cardiology’s Statin Intolerance Tool (launched March 2023)-free for clinicians, helps calculate risk vs. benefit
Wait times can be long-6 to 8 weeks in some places. But if you’ve been told you can’t take statins and you’re still at risk for a heart attack, it’s worth the wait. Your cholesterol doesn’t wait.
Bottom Line: You’re Not Out of Options
Statin intolerance doesn’t mean you’re stuck with high cholesterol. It means you need a smarter approach. Most people who think they can’t take statins can-once they’re evaluated properly. Structured clinics use proven protocols to get patients back on treatment, reduce side effects, and prevent heart attacks.
Don’t accept a "no" from your doctor. Ask: "Have you ruled out other causes? Have you tried a different statin? Have you considered intermittent dosing?" If the answer is no, ask for a referral. Your heart is worth the effort.


Comments
Andrew Baggley
November 20, 2025 AT 19:00Frank Dahlmeyer
November 22, 2025 AT 12:07Paige Lund
November 22, 2025 AT 18:56Reema Al-Zaheri
November 23, 2025 AT 00:22Derron Vanderpoel
November 23, 2025 AT 06:37Codie Wagers
November 24, 2025 AT 23:52Timothy Reed
November 25, 2025 AT 05:15Michael Salmon
November 26, 2025 AT 03:12Michael Petesch
November 27, 2025 AT 13:31Angela Gutschwager
November 28, 2025 AT 02:50Christopher K
November 28, 2025 AT 08:57Joe Durham
November 29, 2025 AT 03:27