It’s one thing to feel a little nauseous after taking a new pill. It’s another when your throat starts closing, your skin peels off, or you can’t breathe. These aren’t side effects - they’re severe adverse drug reactions, and they can kill you in minutes if you wait too long to act.
Every year in the U.S., between 7,000 and 9,000 people die from medication errors and severe drug reactions. Most of these deaths are preventable. The key? Recognizing the warning signs early and acting fast. You don’t need to be a doctor. You just need to know what to look for - and what to do next.
What Counts as a Severe Drug Reaction?
A severe adverse drug reaction isn’t just an unpleasant side effect. The FDA defines it as any reaction that causes death, is life-threatening, requires hospitalization, leads to permanent damage, or causes a disability. That means if a drug makes you sick enough to end up in the ER, it’s serious - even if you didn’t think it was a big deal at first.
Some reactions happen fast. Others creep up over days or weeks. The most dangerous ones fall into four main types:
- Type I (IgE-mediated): These are allergic reactions that hit within minutes to two hours. Think anaphylaxis.
- Type II (Cytotoxic): Your immune system attacks your own blood cells. Can cause severe anemia or low platelets.
- Type III (Immune complex): Symptoms like fever, joint pain, and rash show up 7-14 days after taking the drug. Often mistaken for the flu.
- Type IV (Delayed T-cell): These cause skin conditions like Stevens-Johnson Syndrome (SJS) or Toxic Epidermal Necrolysis (TEN). They can start as a mild rash but turn deadly in days.
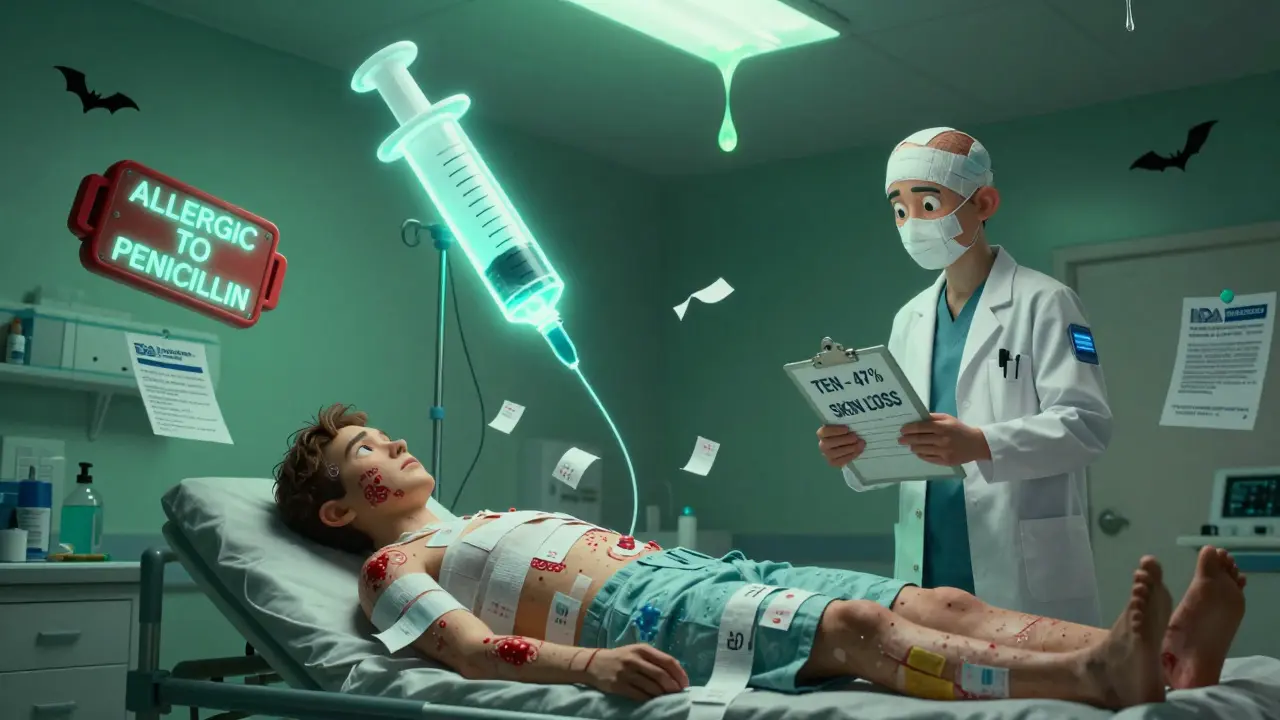
Anticoagulants like warfarin, diabetes drugs like insulin, and opioids like morphine are the top three culprits behind the most serious reactions. But almost any drug - even something as common as penicillin or ibuprofen - can trigger a life-threatening response in someone who’s sensitive.
When You Must Call 911 or Go to the ER
If you’re taking a new medication and you notice any of these symptoms, don’t wait. Don’t text your doctor. Don’t Google it. Get help now:
- Sudden swelling of the lips, tongue, throat, or face
- Wheezing, gasping for air, or feeling like you’re choking
- Rapid heartbeat, dizziness, fainting, or passing out
- A rash that spreads fast, blisters, or causes skin to peel off
- High fever (over 102°F) with a rash, especially if it’s painful or involves the eyes or mouth
- Unexplained bruising, bleeding gums, or dark urine (signs of internal bleeding or organ damage)
These aren’t "maybe" signs. They’re red flags. The Resuscitation Council UK says it clearly: "Initial treatment should not be delayed by a lack of a complete history or definite diagnosis." If you’re unsure, treat it like an emergency.
Anaphylaxis: The Fastest Killer
Anaphylaxis is the most dangerous Type I reaction. It can start with a runny nose or a little itching - then spiral into a full-body collapse in under 10 minutes. You might feel your throat tightening. Your skin might break out in hives. Your blood pressure could crash. You could lose consciousness.
Here’s what to do:
- Use your epinephrine auto-injector immediately. Inject into the outer thigh. Even if you’re not 100% sure - use it. Epinephrine is safe. Waiting is not.
- Call 911. Even if you feel better after the shot, you still need emergency care. Symptoms can come back.
- Lie down and keep still. Elevate your legs if you can. Don’t stand up.
- If you’re alone, use your phone to call for help while injecting. If someone’s with you, have them call and stay with you.
Epinephrine is the only thing that stops anaphylaxis. Antihistamines like Benadryl? They help with itching, but they won’t save your life. Don’t rely on them alone.

Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis: Skin That Melts
These are rare, but deadly. SJS and TEN are Type IV reactions. They start like a bad sunburn or flu - fever, sore throat, burning eyes. Then, within 1-3 days, a painful red rash spreads. Blisters form. Your skin starts peeling off in sheets - sometimes over 30% of your body.
Mortality rates? 10% for SJS. Up to 50% for TEN. The older you are or the more skin you lose, the higher the risk.
What to do:
- Stop the drug immediately. Don’t wait for a doctor’s order.
- Go to the ER. This isn’t a dermatologist appointment. This is a burn unit emergency.
- Don’t try to pop blisters or peel skin. Leave it to the hospital team.
Doctors treat this like a severe burn. You’ll need IV fluids, pain control, and often isolation to prevent infection. Recovery takes weeks - and sometimes leaves permanent scarring or eye damage.
What to Carry If You’re at Risk
If you’ve had a severe reaction before - or if you know you’re allergic to a drug - you need to be prepared:
- Carry an epinephrine auto-injector (EpiPen, Auvi-Q, etc.). Keep it with you at all times. Check the expiration date every few months.
- Wear a medical alert bracelet. List your drug allergies clearly.
- Have a written emergency action plan. Include names of the drugs you react to, symptoms to watch for, and steps to take.
- Train your family, coworkers, or roommates. They might need to use the injector if you can’t.
The American Academy of Family Physicians says: "Epinephrine is the primary treatment for life-threatening allergic reactions." If you don’t have one and you’re at risk, ask your doctor for a prescription. It’s not optional.
What Happens After the Emergency
Once you’re stabilized, the work isn’t over. You’ll need follow-up care:
- See an allergist. They can test you to confirm which drug caused the reaction.
- Get your medical records updated. Every doctor, pharmacist, and ER should know your allergies.
- Ask about alternatives. There’s almost always another drug that won’t trigger the same reaction.
- Report the reaction. Use the FDA’s MedWatch system or ask your doctor to file a report. This helps protect others.
Don’t assume you’ll "outgrow" a severe reaction. Once you’ve had SJS or anaphylaxis from a drug, you’re at high risk of having it again - even with tiny doses.
Common Mistakes People Make
Here’s what goes wrong - and how to avoid it:
- "I’ll wait and see." Delaying epinephrine increases death risk. Every minute counts.
- "I took it before and it was fine." Allergies can develop after one exposure. You don’t need to have had a reaction before to have one now.
- "I used Benadryl and I feel better." That’s a trap. Benadryl doesn’t stop anaphylaxis. It only masks some symptoms.
- "I didn’t think it was serious." A rash that looks "mild" could be the start of TEN. Don’t judge severity by appearance.
Trust your body. If something feels wrong after taking a drug - especially if it’s new or changed - assume it’s serious until proven otherwise.
Final Warning: This Isn’t About Being Scared
It’s about being ready. Medications save lives. But they can also take them - if you don’t know the signs. The goal isn’t to scare you off drugs. It’s to make sure you know when to act.
Carry your epinephrine. Know your allergies. Tell your family. Act fast. You don’t need to be a medical expert. You just need to know that when your body screams for help - you answer.
Can a drug reaction happen days after taking the medicine?
Yes. Some severe reactions, like Stevens-Johnson Syndrome (SJS) or DRESS (Drug Reaction with Eosinophilia and Systemic Symptoms), can take days or even weeks to appear. DRESS often shows up 2-6 weeks after starting a drug and includes fever, rash, and organ inflammation. If you develop a new rash, fever, or swelling after taking a medication - even if it was weeks ago - seek medical help immediately.
Is it safe to use an epinephrine auto-injector if I’m not sure it’s an allergic reaction?
Yes. Epinephrine is very safe for most people, even if they don’t have a true allergy. The risks of not using it during anaphylaxis far outweigh the risks of using it unnecessarily. The Resuscitation Council UK and FDA both state that if there’s any doubt, give epinephrine. It can mean the difference between life and death. Don’t wait for perfect certainty.
Can I take Benadryl instead of epinephrine for a severe reaction?
No. Benadryl (diphenhydramine) helps with itching and hives, but it does not stop the life-threatening drop in blood pressure or airway swelling that comes with anaphylaxis. Only epinephrine can reverse these symptoms. Using Benadryl alone delays proper treatment and increases the risk of death. Always use epinephrine first - then call 911.
Do I need to report a severe drug reaction to anyone?
Yes. Reporting helps protect others. You can report directly to the FDA through their MedWatch program or ask your doctor to file a report. The U.S. Department of Health and Human Services collects these reports to track dangerous drugs and update safety guidelines. Even one report can make a difference in preventing future deaths.
What drugs are most likely to cause severe reactions?
The top three are anticoagulants (like warfarin), diabetes medications (like insulin), and opioids (like morphine). Antibiotics (especially penicillin and sulfa drugs), NSAIDs (like ibuprofen), and seizure medications (like carbamazepine) are also common triggers. But any drug can cause a severe reaction in the right person - especially if you’ve had a reaction before.


Comments
Prateek Nalwaya
February 16, 2026 AT 05:47Man, this post hit different. I’ve been on antibiotics for years and never thought about how one little pill could turn my skin into a melting candle. Had a buddy once get SJS from a sulfa drug - he was in the ICU for 3 weeks, lost 40% of his epidermis. They said if he’d waited another 6 hours, he wouldn’t have made it. Scary as hell. Now I carry my EpiPen like it’s my phone. No joke.
Jonathan Ruth
February 16, 2026 AT 12:09Oliver Calvert
February 17, 2026 AT 07:01Haley DeWitt
February 18, 2026 AT 18:45John Haberstroh
February 20, 2026 AT 03:24So I took a Zpack last year and got this weird rash that looked like a spiderweb. I thought it was heat. Took Benadryl. It faded. Two weeks later I got the same rash - worse. This time I didn't mess around. Went to urgent care. Turns out it was DRESS. My liver was inflamed. I spent 4 days hooked to IVs. They said I was lucky. I wasn't lucky. I was just stupid. Now I have a medical bracelet. And I scream 'NO PENICILLIN' at every pharmacist. Don't be me.
Carrie Schluckbier
February 21, 2026 AT 16:20Liam Earney
February 23, 2026 AT 06:41Oh my god. I just read this and I’m crying. Not because I’m dramatic - though I am - but because I lost my cousin to this. She was 24. Took a new painkiller for her back. Said it was ‘just a rash.’ She didn’t have an EpiPen. She didn’t know the signs. They told her to ‘wait and see.’ She died three days later. I still have her hospital bracelet. I wear it every day. Please. If you’re reading this. Please. Carry it. Tell someone. Don’t wait. I beg you.
guy greenfeld
February 24, 2026 AT 10:09What if the real danger isn't the drug... but the idea that we can control biology with chemistry? We think we’re smart because we invented pills. But the body? It remembers. It retaliates. That rash? That fever? That’s not a side effect. It’s the body screaming: ‘I am not a machine.’ We treat symptoms like bugs to be fixed. But maybe - just maybe - we’re the ones who need to change. Not the medicine. Not the dosage. Us.
Adam Short
February 24, 2026 AT 10:45Sam Pearlman
February 25, 2026 AT 07:08Steph Carr
February 25, 2026 AT 18:13