Organ Rejection Cost Calculator
Understand the Financial Impact
Organ rejection adds 15-30% to transplant costs. The calculator below estimates the financial impact of rejection episodes and potential savings from prevention strategies.
Cost Analysis Results
Baseline Costs
Transplant cost: AUD 70,000
Annual immunosuppression: AUD 1,500
Rejection Impact
Rejection episode cost: AUD 28,000
Additional annual immunosuppression: AUD 0
Potential Savings
With optimized prevention strategies:
This represents a potential 15% reduction in total costs.
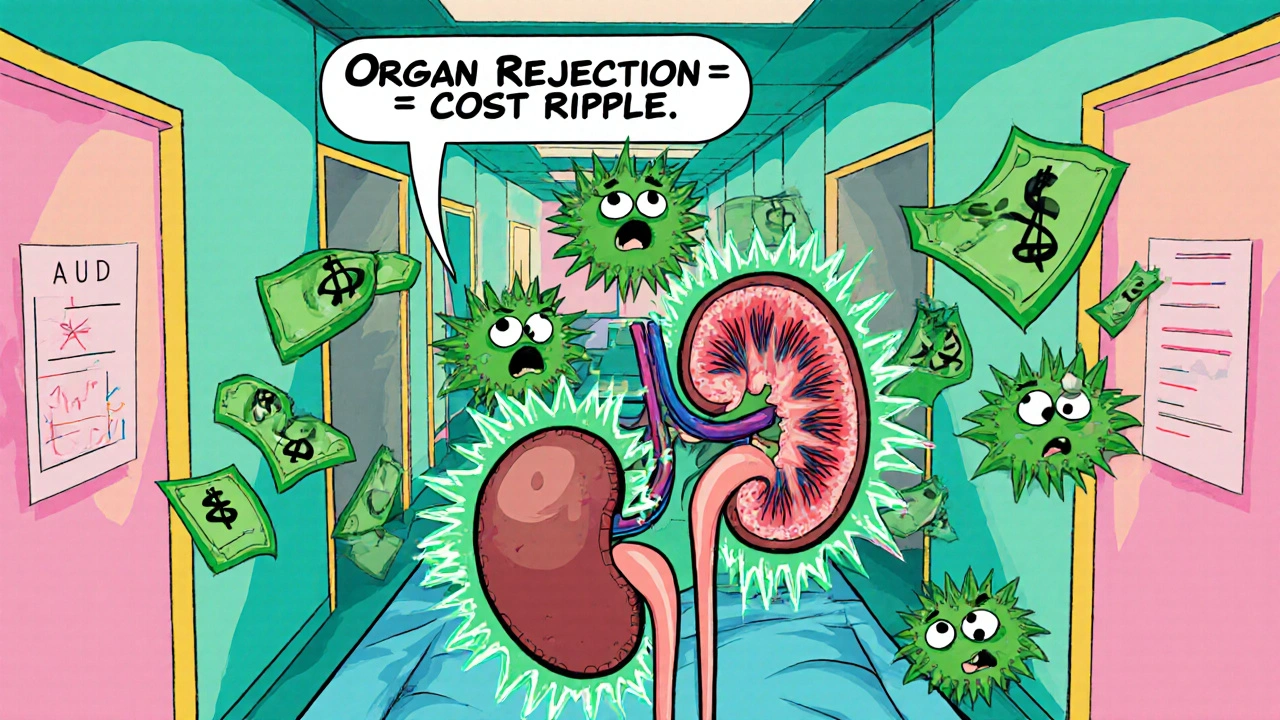
When a transplanted organ is recognized as foreign, organ rejection is the immune‑mediated attack that can compromise graft function and drive up medical costs. The ripple effect reaches hospitals, insurers, and taxpayers, especially in systems like Australia’s Medicare where transplant funding is tightly regulated. Understanding the financial ripple helps policymakers and clinicians target the right interventions.
Key Takeaways
- Organ rejection adds roughly 15‑30% to the total cost of a transplant episode.
- Acute rejection episodes are the biggest cost drivers, often requiring hospital readmission and expensive drugs.
- Chronic rejection leads to graft loss, triggering re‑transplantation or dialysis, which dramatically raises long‑term expenses.
- Effective immunosuppressive therapy and early monitoring can cut costs by up to 25%.
- Funding models that bundle post‑transplant care see better resource allocation than fee‑for‑service structures.
How Organ Rejection Happens
After a kidney transplantation the surgical placement of a donor kidney into a recipient, the recipient’s immune system may launch an attack if the donor’s human leukocyte antigens (HLA) don’t match closely enough. This response is categorized as acute rejection a rapid immune response occurring days to weeks after surgery or chronic rejection a slow, progressive loss of graft function over months or years. Both types demand medical intervention, but their cost profiles differ sharply.
Direct Medical Costs of Rejection
The most visible expense is hospital readmission. A 2023 Australian study found the average cost of an acute kidney rejection admission to be AUD 28,000, compared with AUD 22,000 for a routine post‑op stay. For liver transplantation surgical replacement of a diseased liver with a donor organ, acute rejection can push the bill above AUD 45,000 due to intensive care stays and specialized imaging.
Immunosuppressive therapy is another major line item. Calcineurin inhibitors (e.g., tacrolimus) and mTOR inhibitors cost roughly AUD 1,200-1,800 per month per patient. If an acute rejection flare occurs, clinicians may add high‑dose steroids or switch to biologics like basiliximab, which can double drug spending for that episode.
| Organ | Baseline Transplant Cost | Acute Rejection Cost | Chronic Rejection Cost |
|---|---|---|---|
| Kidney | 70,000 | 28,000 | 120,000 (including dialysis) |
| Liver | 130,000 | 45,000 | 200,000 (including re‑transplant) |
| Heart | 150,000 | 55,000 | 250,000 (including ventricular assist device) |
Indirect Costs and Resource Strain
Beyond the hospital bill, rejection episodes sap productivity and increase caregiver burden. A 2022 economic analysis estimated that each acute rejection event adds roughly 12 weeks of lost work time for the patient and 8 weeks for a primary caregiver. In Australia’s universal health system, these lost wages translate to lower tax revenues and higher social support payouts.
Long‑term, chronic rejection forces patients back onto dialysis or onto the organ‑waiting list, inflating the demand for dialysis centers and organ procurement organizations (OPOs). The Australian OPO network reports a 7% annual rise in dialysis slots linked directly to graft failure.
Funding Challenges for Health Systems
National health budgets allocate funds based on projected procedure volumes and average costs. When rejection rates climb, actual expenditures overshoot forecasts, creating budget gaps. Medicare’s Medicare Benefits Schedule (MBS) accounts for baseline transplant surgery but only partially reimburses post‑transplant monitoring, leaving hospitals to absorb excess costs.
Private insurers face similar dilemmas. They must balance premium affordability with coverage for costly biologic agents used in refractory rejection. In many cases, pre‑authorization delays lead to worse clinical outcomes and higher downstream spending.
Strategies to Reduce the Financial Burden
Investing in better prevention pays off. Here are proven approaches:
- Enhanced HLA Matching: Using high‑resolution typing reduces acute rejection rates by up to 15%.
- Therapeutic drug monitoring (TDM) of tacrolimus keeps blood levels within target range, cutting rejection episodes by 20%.
- Adopting protocol biopsies for early detection catches subclinical rejection before it becomes costly.
- Exploring tolerance‑inducing protocols, such as donor‑derived regulatory T‑cell infusions, shows promise in reducing lifelong immunosuppression.
- Bundled payment models that include 12‑month post‑transplant care incentivize hospitals to keep rejection low.
The financial impact of organ rejection can be mitigated when health systems align clinical pathways with cost‑containment incentives.
Policy Implications and Future Outlook
Policymakers need reliable data to adjust funding formulas. Integrating transplant registries with national health expenditure databases enables real‑time cost tracking. Moreover, expanding coverage for newer, less toxic immunosuppressants could lower long‑term graft loss, ultimately saving money.
Australia’s recent investment in the National Organ Donation and Transplantation Registry (NODTR) aims to provide the analytics needed for evidence‑based budgeting. As more granular cost data become available, we can expect more nuanced reimbursement tiers that reflect the true cost of rejection prevention versus treatment.
Checklist for Clinicians and Administrators
- Implement high‑resolution HLA typing for every donor‑recipient pair.
- Standardize therapeutic drug monitoring protocols for calcineurin inhibitors.
- Schedule protocol biopsies at 3, 6, and 12 months post‑transplant.
- Use bundled payment contracts that cover immunosuppressive drugs and follow‑up visits.
- Report all rejection episodes to the national registry within 30 days.
Frequently Asked Questions
What is the difference between acute and chronic organ rejection?
Acute rejection occurs days to weeks after transplantation and is usually reversible with intensified immunosuppression. Chronic rejection develops over months or years, leading to progressive loss of graft function and often requiring re‑transplant or dialysis.
How much does a typical rejection episode cost in Australia?
For a kidney transplant, an acute rejection admission averages around AUD 28,000, while chronic rejection that leads to dialysis can exceed AUD 120,000 over the course of a year.
Can better HLA matching really reduce costs?
Yes. Studies show that high‑resolution HLA matching cuts acute rejection rates by 15% and saves roughly AUD 4,000-6,000 per transplant by avoiding expensive hospital readmissions.
What role do immunosuppressive drugs play in the financial picture?
Immunosuppressants are a double‑edged sword: they prevent rejection but are costly themselves. Optimizing dosing through therapeutic drug monitoring can lower both drug spend and the risk of costly rejection episodes.
How do bundled payment models affect transplant budgeting?
Bundled payments combine surgery, post‑operative care, and immunosuppressive therapy into a single reimbursement. This incentivizes hospitals to keep rejection rates low, aligning clinical quality with financial sustainability.

Comments
Sarah Riley
October 22, 2025 AT 20:52The immunologic allorecognition cascade imposes a quantifiable externality on the health‑economic equilibrium. Consequently, marginal cost functions for transplant programs exhibit an upward shift proportional to rejection incidence.
Benedict Posadas
October 28, 2025 AT 14:45Wow, this post really opened my eyes on how pricey rejection can be! 🤩 Hospitals gotta spend big bucks on readmissions, and patients end up worrying about meds and bills. We need more proactive monitoring, maybe some AI alerts, so we catch issues early. Also, if insurers speed up pre‑auth, outcomes improve big tim! Let’s keep pushing for smarter funding models 😊
Kiara Gerardino
November 3, 2025 AT 09:39It is an egregious moral failure that our societies permit such wastage of resources on preventable graft loss. The complacent bureaucracy must be held accountable for the needless suffering of patients.
Tim Blümel
November 9, 2025 AT 04:32From a systems perspective, every rejection episode reverberates through the macro‑allocation of healthcare capital. By integrating real‑time biomarker analytics, clinicians can preemptively modulate immunosuppression, thereby curbing downstream costs. Moreover, patient empowerment through education fosters adherence, which is a cornerstone of graft longevity. 🌱
Harini Prakash
November 14, 2025 AT 23:25I totally agree with your point about real‑time analytics, Tim. In practice, implementing such tools requires collaborative budgeting between hospitals and payers. 😊
Diane Thurman
November 20, 2025 AT 18:19Honestly, if hospitals kept their budgets in check, they wouldn't have this problem.
Sameer Khan
November 26, 2025 AT 13:12The fiscal ramifications of alloimmune-mediated graft injury demand rigorous econometric modeling to inform sustainable reimbursement schemas.
Empirical evidence demonstrates that acute rejection episodes inflate direct hospital expenditures by approximately 18 % relative to uncomplicated transplants.
When extrapolated across national transplant volumes, this incremental cost translates into a multibillion‑dollar burden on the public purse.
A pivotal lever for mitigation resides in the preemptive optimization of HLA compatibility via high‑resolution genotyping.
Such precision matching has been correlated with a 12‑15 % reduction in acute rejection incidence.
Consequently, the marginal cost per transplant declines, effecting downstream savings in both pharmaceutical outlays and inpatient care.
Parallelly, therapeutic drug monitoring protocols for calcineurin inhibitors enhance pharmacodynamic targeting, curbing both under‑ and over‑exposure.
The resultant attenuation of immunologic flare‑ups diminishes the need for costly rescue biologics.
From a macroeconomic standpoint, reduced readmission rates alleviate pressure on bed capacity, thereby improving overall health system throughput.
Furthermore, integrating transplant registry data with national health expenditure databases facilitates real‑time cost attribution.
This data fusion enables policymakers to calibrate bundled payment structures that encapsulate the full continuum of post‑transplant care.
Such bundled models incentivize providers to invest in preventive interventions, aligning clinical quality with fiscal responsibility.
In jurisdictions where bundled payments have been piloted, preliminary analyses reveal a 9 % contraction in total episode cost.
Nevertheless, successful implementation necessitates robust contractual frameworks that delineate risk sharing between payers and providers.
Equally essential is the establishment of transparent reporting standards for rejection events to ensure actuarial accuracy.
In sum, a synergistic approach that melds high‑resolution immunogenetics, pharmacokinetic stewardship, and data‑driven financing will sustainably attenuate the economic toll of organ rejection.
WILLIS jotrin
December 2, 2025 AT 08:05Your comprehensive breakdown crystallizes the path forward. The interplay between precision medicine and fiscal policy is indeed the linchpin for durable transplant ecosystems. It will be interesting to see how stakeholder alignment evolves as these models mature. 🤔