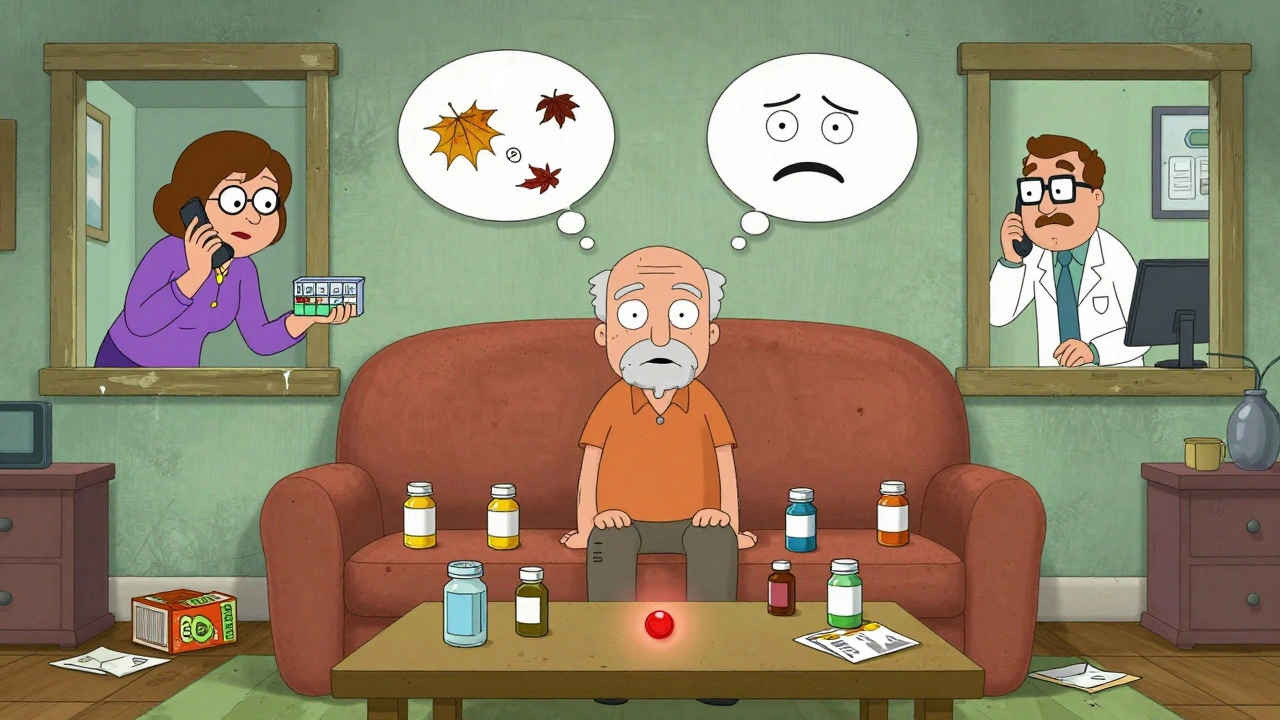
More than 88% of adults over 65 take at least one prescription drug. Nearly half take five or more. And yet, nearly half of them don’t take them as prescribed. This isn’t laziness. It’s not forgetfulness alone. It’s a tangled mess of physical limits, financial stress, confusing routines, and systems that don’t keep up with aging bodies.
Why Do Seniors Skip Their Meds?
It’s not one problem. It’s five big ones, all piled on top of each other.Polypharmacy - taking four, five, or even ten pills a day - is the biggest trigger. Imagine having to remember to take six different pills at three different times. One for blood pressure, one for diabetes, one for cholesterol, two for pain, maybe a vitamin. Each has its own rules: take with food, take on empty stomach, don’t lie down for 30 minutes. It’s overwhelming. Studies show people taking just one pill a day are far more likely to stick with it than those juggling multiple doses.
Cognitive changes make it worse. Memory fades. Time blurs. A pill might look like another. A bottle might be opened but never finished. Older adults often don’t realize they’ve missed a dose until days later. Some even stop taking meds because they feel fine - not understanding that the drug is what’s keeping them fine.
Physical limits get in the way too. Arthritis makes opening childproof caps hard. Vision fades, so tiny print on labels becomes unreadable. Hands shake, so pills spill. Some seniors skip doses because they can’t physically open the bottle or read the instructions.
Cost is a silent killer. One in three older adults who can’t afford their meds cut back, delay refills, or skip doses. Women, Black, and Hispanic seniors face higher rates of cost-related nonadherence. Food insecurity makes it worse: if you have to choose between insulin and dinner, you’ll choose dinner. The CDC found food-insecure seniors are six times more likely to skip meds because of cost.
Social isolation is the hidden driver. Many seniors live alone. No one checks if they took their pills. No one notices when they stop refilling prescriptions. Family may live far away. Friends may not know what to ask. Without someone to notice, a missed dose becomes a missed week, then a missed month.
What Actually Helps? Real Fixes, Not Just Ideas
Solutions don’t need fancy tech. They need simplicity, consistency, and human connection.Simplify the regimen. Ask the doctor: Can we cut any pills? Can we switch to once-daily versions? Can we combine two meds into one pill? Many seniors take two separate drugs for the same condition - like two different blood pressure pills. Merging them into a single tablet cuts the daily count in half. That’s not just convenient - it’s life-changing. One study showed adherence jumped from 52% to 81% when complex regimens were streamlined.
Use pill organizers - the right way. Not just any box. Use ones with alarms, clear labels, and separate compartments for morning, afternoon, evening, and night. Look for models with lock lids to prevent accidental overdose. Some even send alerts to family members if a dose is missed. Don’t just hand a senior a plastic box and walk away. Set it up together. Fill it weekly. Check in every Sunday.
Bring in the pharmacist. Pharmacists are underused. They’re the ones who see every prescription a patient fills. Ask for a medication therapy review. It’s free under Medicare. The pharmacist checks for duplicates, interactions, unnecessary drugs, and confusing instructions. They can repackage pills into easy-open blister packs. They can even call your doctor to suggest changes.
Make it visual and audible. Put a sticky note on the fridge: “Take Amlodipine with breakfast.” Use a digital clock with a voice reminder: “It’s 8 a.m. Time for your heart pill.” Smart speakers like Amazon Echo can be programmed to give daily reminders. No smartphone? No problem. A simple alarm clock with a voice feature works too.
Build in social support. If a neighbor, church volunteer, or home care aide can drop by once a week to check the pill box, adherence improves dramatically. Even a weekly phone call from a family member asking, “Did you take your pills today?” makes a difference. One study found seniors with daily check-ins were 40% more likely to stay on track.
Reduce out-of-pocket costs. If a senior can’t afford a $500 monthly drug, no reminder system will help. Ask about patient assistance programs. Many drug makers offer free or low-cost meds to low-income seniors. Use GoodRx to compare prices across pharmacies. Ask if a generic version exists. Switching from brand-name Lisinopril to generic can cut the cost from $120 to $4 a month.
What Doesn’t Work - and Why
Not every solution fits. Avoid these common traps.Apps and smart watches sound great - but many seniors don’t use smartphones. If they do, they may not know how to set reminders or navigate the app. A 78-year-old with arthritis won’t tap a screen to log a pill. Simplicity wins.
Written instructions on tiny labels? Useless if vision is poor. Large-print labels or voice-readers are better.
Blaming the patient for “not being responsible” ignores the real barriers. A senior who skips a pill isn’t being stubborn - they’re overwhelmed, confused, or broke. The system failed them, not the person.
One-time education - like a pamphlet at discharge - doesn’t stick. Medication understanding needs reinforcement. A single talk with a nurse won’t change behavior. Weekly check-ins will.
When Things Go Wrong - Signs to Watch For
Sometimes, non-adherence shows up in strange ways. A senior might fall more often. They might seem more confused. They might have sudden dizziness or urinary incontinence. These aren’t just signs of aging - they could be side effects of missed or wrongly taken meds.Watch for:
- Empty pill bottles that haven’t been refilled
- Pills stacked in a drawer or on a nightstand
- Unexplained falls or confusion
- Doctor visits for symptoms that are actually drug-related
- Reluctance to talk about meds - “I’m fine,” “I don’t need them,” “I took them”
If you notice any of these, don’t accuse. Ask gently: “I noticed your blood pressure pills haven’t been refilled. Is there a reason?” Then listen.
How Caregivers Can Help - Without Taking Over
You don’t need to be a nurse to make a difference.- Go with them to one doctor visit. Take notes. Ask: “Can we simplify this?”
- Help refill prescriptions before they run out. Set calendar alerts.
- Call the pharmacy and ask if they offer home delivery or free medication packaging.
- Check the fridge. Are the pills still there? Are they expired?
- Don’t assume they know what each pill does. Ask them to explain it back to you.
The goal isn’t control. It’s partnership. Let them keep their dignity. Just help remove the roadblocks.
The Bigger Picture: Why This Matters
Skipping meds isn’t just about a headache or a missed dose. It’s about hospital stays, emergency rooms, and early death. The NIH estimates medication non-adherence causes 200,000 preventable deaths in the U.S. every year - more than car crashes. For seniors with heart disease, diabetes, or kidney problems, missing even one dose can trigger a crisis.Healthcare systems are starting to notice. Medicare now tracks adherence rates. Pharmacies get paid more when patients stay on their meds. But real change happens at home - in the kitchen, at the dinner table, during a weekly phone call.
Medications don’t work if they’re not taken. And for older adults, taking them isn’t just about health - it’s about independence, dignity, and the quiet hope of staying in their own home a little longer.
Why do older adults forget to take their medications?
Forgetting isn’t just about memory loss. It’s often due to complex regimens - multiple pills at different times - combined with vision problems, hearing loss, or lack of daily structure. Many seniors don’t realize they’ve missed a dose until days later. Simple reminders, pill organizers, and weekly check-ins help more than trying to rely on memory alone.
Can cost really make someone skip life-saving meds?
Yes. Nearly 4% of seniors skip doses because they can’t afford them. For food-insecure seniors, that number jumps to six times higher. Some cut pills in half, delay refills, or stop taking them entirely. Generic versions, patient assistance programs, and pharmacy discount cards like GoodRx can reduce costs dramatically - sometimes from $100 to under $5 per month.
What’s the best way to organize pills for an older adult?
Use a weekly pill organizer with separate compartments for morning, afternoon, evening, and night. Choose one with alarms or that connects to a smartphone app. Some models have lock lids and send alerts to caregivers if a dose is skipped. Fill it together once a week. Don’t just hand it over - make it part of a routine, like Sunday lunch.
Should I talk to the doctor about reducing my parent’s medications?
Absolutely. Many seniors take drugs that are no longer needed or that interact dangerously. Ask for a medication review - it’s free under Medicare. The doctor can check for duplicates, unnecessary prescriptions, or drugs with side effects that mimic aging. Cutting even one or two pills can improve safety and adherence.
Are there free resources to help seniors manage their meds?
Yes. Medicare offers free Medication Therapy Management (MTM) through pharmacies. Local Area Agencies on Aging often provide free home visits to help with pill organization. Pharmacies like CVS and Walgreens offer free blister packs and home delivery. GoodRx gives discounts on prescriptions. And many drug makers offer free or low-cost programs for low-income seniors.
How do I know if my parent is hiding their non-adherence?
Look for signs: empty bottles that haven’t been refilled, pills stacked in drawers, unexplained falls or confusion, or vague answers when asked about meds. Don’t confront. Ask open-ended questions: “I noticed your blood pressure pills haven’t been refilled. Is there a reason?” Listen. Often, the answer is cost, fear of side effects, or feeling overwhelmed.
What to Do Next
Start small. Pick one thing:- Call the pharmacy and ask if they offer free blister packs or home delivery.
- Set up a weekly phone call or visit to check the pill box.
- Ask the doctor for a medication review - even if the senior says they’re fine.
- Use GoodRx to check if a cheaper generic version exists.
- Write down the name, purpose, and time of each pill and tape it to the fridge.
Adherence isn’t about perfection. It’s about progress. One less pill. One reminder. One less trip to the ER. That’s how you help someone stay healthy - and stay home - a little longer.


Comments
Joe Lam
December 4, 2025 AT 00:49Let’s be real - this whole article reads like a corporate whitepaper written by someone who’s never met a senior who actually takes 12 pills a day. You talk about ‘simple solutions’ like pill organizers, but have you ever tried to get someone with Parkinson’s to open a childproof cap while their hands shake like a maraca? Or explain to a widow who lost her husband last year why she needs to take a pill she doesn’t even remember the name of? This isn’t a logistics problem - it’s a societal failure dressed up as a checklist.
jagdish kumar
December 5, 2025 AT 18:52Medication is just another illusion of control. We take pills to pretend we can outsmart death. But the body remembers what the mind forgets. The real question isn’t how to make them take it - it’s why we think they should.
zac grant
December 5, 2025 AT 20:28From a clinical perspective, this is textbook polypharmacy management 101 - and honestly, the interventions listed are among the most evidence-backed in geriatric pharmacotherapy. The key is system-level integration: MTM (Medication Therapy Management) under Medicare Part D has shown 22-34% adherence improvement in RCTs when paired with pharmacist-led reconciliation. Blister packs + weekly check-ins + voice-activated reminders? That’s a multi-modal behavioral nudge framework. It works because it reduces cognitive load, not because it’s ‘nice.’
Pavan Kankala
December 7, 2025 AT 05:53Of course they’re skipping meds. The system wants them sick. More prescriptions = more profits. The FDA, Big Pharma, and Medicare all profit when seniors are on 8 drugs, not 2. They don’t want you to simplify - they want you dependent. That ‘free’ MTM? It’s a trap. They track your data, sell it, then upsell you more pills next year. Read the fine print. This isn’t help - it’s surveillance with a smile.
Jessica Baydowicz
December 7, 2025 AT 18:35Y’all. I just got my 82-year-old aunt set up with a pill organizer that beeps AND texts me if she misses a dose. She thought it was a robot but now she calls it ‘Buddy’ and talks to it like a grandkid. We did it over pizza. She cried. I cried. We’re not fixing the system - we’re building tiny moments of love around it. And guess what? She’s taking her meds now. No magic. Just presence. 💛
John Filby
December 9, 2025 AT 04:27Just had this convo with my dad last week - he’s been skipping his statin because he ‘feels fine.’ I printed out a big label with his meds, why he takes them, and the time, and stuck it on the fridge next to the milk. He laughed and said, ‘You turned my kitchen into a pharmacy.’ But he took it this morning. Small wins, folks. Also, GoodRx saved us $98 on his blood pressure med. 🙌
Rachel Bonaparte
December 9, 2025 AT 18:48Let’s not pretend this is about health. This is about control. The medical-industrial complex has turned aging into a revenue stream. Pills are the new pacifiers. They don’t care if you live - they care if you keep buying. And the ‘simple solutions’? They’re distractions. The real fix is universal healthcare with mandatory geriatric pharmacists in every clinic - not some sticky note on the fridge. This article is a Band-Aid on a hemorrhage, wrapped in virtue signaling and free GoodRx coupons. Don’t be fooled. The system is rigged. And they’re counting on you to blame the patient, not the profit motive.
Scott van Haastrecht
December 11, 2025 AT 06:54Here’s the truth no one wants to say: most of these seniors are dying anyway. The real cost isn’t the pills - it’s the ER visits, the nursing homes, the family burnout. Why are we pouring resources into keeping people alive longer when their quality of life is already gone? This isn’t compassion - it’s guilt-driven over-medicalization. Let them go with dignity. Stop forcing pills on people who just want to sleep.