For someone living with type 1 diabetes, managing blood sugar every single day can feel like a full-time job. Injections multiple times a day, counting carbs, checking glucose levels, adjusting doses - it never stops. That’s why so many people turn to insulin pump therapy. It’s not a cure, but for many, it changes everything. Instead of needles, you wear a small device that delivers insulin continuously. No more lunchtime injections at work. No more waking up in the middle of the night to check your sugar. But it’s not magic. There are real downsides, technical hurdles, and it takes work to make it fit your life.
What Exactly Is an Insulin Pump?
An insulin pump is a small, wearable device - about the size of a smartphone - that delivers rapid-acting insulin through a thin tube or patch stuck under your skin. It doesn’t replace insulin; it just gives it to you differently. Instead of injecting long- and short-acting insulin separately, the pump only uses rapid-acting insulin, delivered in two ways: a steady background dose (called basal insulin) and extra doses (boluses) when you eat or correct high blood sugar.Modern pumps are smarter than ever. Many connect to continuous glucose monitors (CGMs) and can automatically adjust insulin delivery based on your real-time sugar levels. These are called hybrid closed-loop systems, or sometimes "artificial pancreas" systems. Brands like Medtronic MiniMed 780G, Tandem t:slim X2 with Control-IQ, and Insulet Omnipod 5 are the most common in the U.S. and Australia. The Omnipod 5 is tubeless - it sticks directly to your skin like a patch - while others have thin tubing that connects to your infusion site.
These devices can deliver insulin in tiny increments - as small as 0.01 units - which is crucial for fine-tuning control. Most pumps hold between 140 to 300 units of insulin, and the reservoir needs replacing every 2 to 3 days. The infusion set (the part under your skin) also needs changing every 2 to 3 days, usually on the abdomen, thigh, or arm.
Why People Choose Insulin Pump Therapy
The biggest reason people switch? Better blood sugar control. A 2022 study of over 25 clinical trials found that pump users had an average HbA1c of 8.3%, compared to 9.2% for those on multiple daily injections. That’s a 0.37% drop - which might sound small, but it translates to fewer long-term complications like nerve damage, kidney issues, and vision loss.Another major win: fewer low blood sugar episodes, especially at night. Nocturnal hypoglycemia is scary - waking up drenched in sweat, confused, or worse. Pump users saw a 32% reduction in these events. Why? Because pumps can be programmed to reduce insulin automatically when glucose levels start to drop. Systems like Medtronic’s Predictive Low Glucose Suspend and Tandem’s Control-IQ can stop insulin delivery before your sugar crashes.
Flexibility is a huge draw. Want to sleep in? Eat dinner at 9 p.m.? Go for a run without planning your insulin timing? With a pump, you can adjust your basal rate on the fly. No more rigid meal schedules. Many users say they feel less like they’re living with diabetes and more like they’re just living.
Surveys from the T1D Exchange show 82% of pump users report improved quality of life. One Reddit user wrote: "My overnight lows dropped from 3-4 times a week to maybe once a month since switching to Omnipod 5." That’s not hype - it’s real life.
The Real Downsides of Insulin Pump Therapy
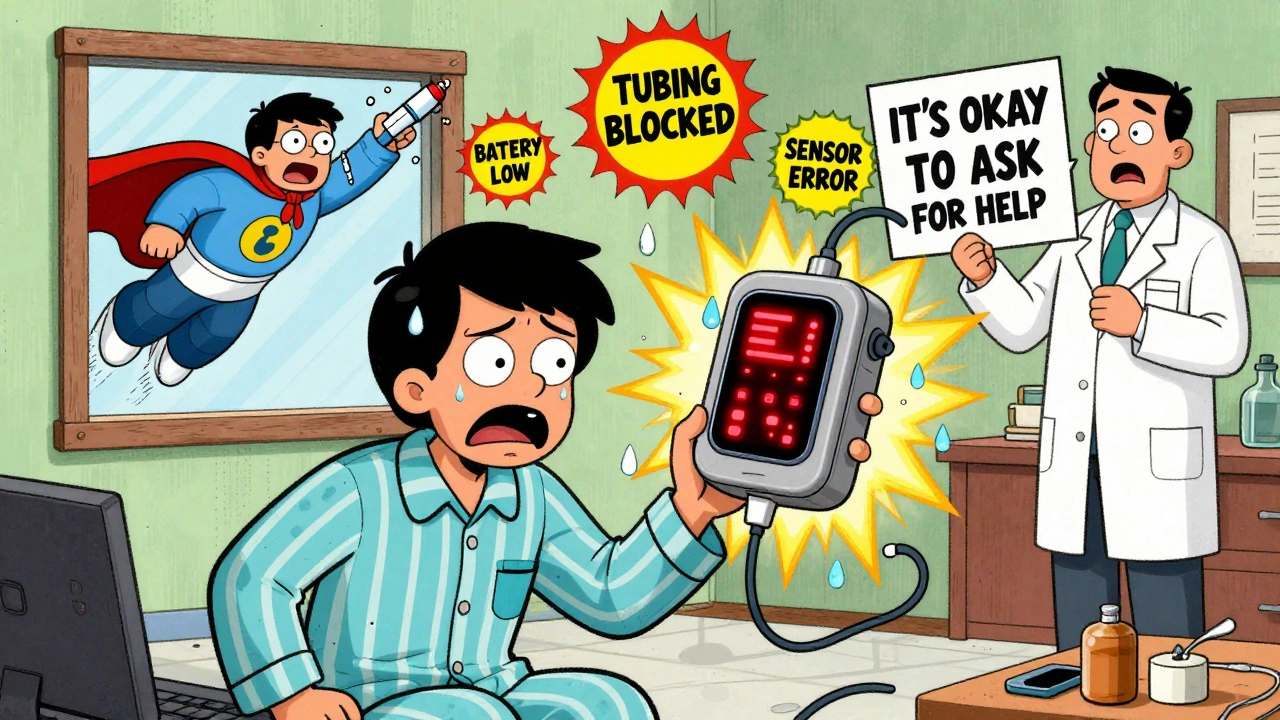
It’s not all smooth sailing. The biggest fear? Insulin delivery failure. If your tubing kinks, your pod falls off, or your pump battery dies, you stop getting insulin. That can lead to diabetic ketoacidosis (DKA) - a dangerous, life-threatening condition - within just 4 to 6 hours. T1D Exchange data shows about 15% of pump users experience an interruption like this at least once a month. That’s why every pump user needs to carry fast-acting insulin pens as backup. Always.Then there’s the tech overload. Pumps beep. They flash. They alert you about low battery, low insulin, blocked tubing, sensor errors. Alarm fatigue is real. One survey found 38% of users feel overwhelmed by constant alerts. Some people turn off alarms - which is dangerous.
Skin irritation is another common issue. About 45% of users report redness, itching, or bumps at the infusion site. Some people just can’t tolerate the adhesive. Others struggle with the tubing getting caught on doors, chairs, or during exercise. The Omnipod’s tubeless design helps here, but it’s not perfect - the patch can peel off during swimming or sweating.
And let’s talk about cost. A new pump runs $5,000 to $7,000. Annual supplies - infusion sets, reservoirs, sensors - cost $3,000 to $5,000. In the U.S., most insurance covers it, but in Australia, coverage varies. Some people pay hundreds out of pocket. If your insurance denies coverage, you’re stuck with injections.

Who Is a Good Candidate for an Insulin Pump?
Not everyone needs or should use a pump. The American Diabetes Association and the Association of Diabetes Care & Education Specialists say pumps are best for people who:- Have high blood sugar variability - glucose levels swinging wildly up and down
- Experience frequent or severe low blood sugar, especially at night
- Have hypoglycemia unawareness - no warning signs when sugar drops
- Have an HbA1c above 7.5% despite trying multiple daily injections
- Want more flexibility in eating, sleeping, or exercising
Children as young as 2 can use pumps, and adoption is higher in kids than adults - 45% of pediatric patients in the U.S. use them. That’s because parents can manage the tech, and kids benefit from fewer injections.
But if you have trouble with fine motor skills, can’t read small screens, forget to check your glucose, or feel anxious around technology, a pump might make things harder. People with eating disorders or severe anxiety about tech often struggle too. It’s not a one-size-fits-all solution.
How to Get Started: The Real Process
Getting a pump isn’t like ordering a new phone. It’s a medical decision that requires education, planning, and support. Here’s what actually happens:- Meet with your diabetes care team. You’ll need a referral from your endocrinologist or GP. They’ll review your history, HbA1c, hypoglycemia episodes, and your ability to manage tech.
- Choose your pump. Your provider will help you pick based on your lifestyle. Want waterproof? Go for Omnipod 5. Want tighter automation? Try Medtronic or Tandem. Insurance often limits your options.
- Get trained. You’ll need 3 to 5 sessions with a certified diabetes educator. You’ll learn how to insert the infusion set, program basal rates, calculate boluses, troubleshoot errors, and handle emergencies. This isn’t a one-hour demo - it takes weeks.
- Start with a trial. Some clinics let you borrow a pump for a few days to test it out. Others start you on a low basal rate and slowly adjust.
- Switch over. You’ll stop your long-acting insulin and start the pump. The first few days are messy. You’ll have highs, lows, and confusion. That’s normal.
- Keep monitoring. You still need to check your glucose 4 to 6 times a day - or use a CGM. Pumps aren’t set-and-forget. The ADA says it clearly: "Pump therapy requires ongoing self-management education."
Most people take 2 to 3 weeks to feel comfortable. Common early problems: misplacing the infusion site (42% of new users), miscalculating carb ratios (35%), and ignoring alarms (28%). Don’t rush. Ask questions. Call your educator if something feels off.
What’s Next for Insulin Pump Tech?
The future is getting even smarter. In early 2023, the FDA approved the Tandem t:slim X2 for kids as young as 2. Medtronic’s MiniMed 880G - expected late 2024 - will extend its safety pause during lows from 60 to 150 minutes. And the Beta Bionics iLet Bionic Pancreas, currently in final trials, doesn’t even need you to enter carb counts. You just plug in insulin and glucagon, and it figures out the rest.By 2027, experts predict 65% of newly diagnosed children in the U.S. will start on a hybrid closed-loop system. That’s up from 32% in 2022. The market is growing fast - projected to hit $8.7 billion by 2029.
But technology doesn’t fix everything. A 2022 study found 12.3% of pump users quit within two years - mostly because of skin issues, alarm fatigue, or just not fitting the lifestyle. So while the tech is advancing, the human part - staying consistent, managing stress, knowing when to ask for help - still matters most.
Is It Right for You?
Ask yourself these questions:- Do I check my blood sugar regularly, even when I feel fine?
- Can I handle a device that beeps, alerts, and sometimes fails?
- Am I willing to carry backup insulin and syringes at all times?
- Do I want more freedom in my meals and schedule?
- Am I okay with the cost and insurance paperwork?
If you answered yes to most of these, a pump could be a game-changer. If you’re unsure, talk to someone who’s been using one for a year. Join a support group. Read real user stories - not just ads.
Insulin pump therapy isn’t about being perfect. It’s about finding a system that lets you live your life without constantly fighting your diabetes. For many, it does exactly that. For others, injections still work better. There’s no shame in either choice. The goal isn’t to use the latest tech - it’s to stay healthy, safe, and in control.
Can kids use insulin pumps?
Yes. Modern insulin pumps like the Omnipod 5 and Medtronic MiniMed 780G are FDA-approved for children as young as 2 years old. Many pediatric endocrinologists recommend pumps for kids because they reduce nighttime lows, improve HbA1c, and make it easier for parents to manage insulin delivery without multiple daily injections. Pumps are especially helpful for young children who can’t communicate low blood sugar symptoms.
Do I still need to check my blood sugar if I use a pump?
Yes. Even with a pump connected to a CGM, you still need to verify your glucose levels with a fingerstick at least once a day - or more if your CGM readings don’t match how you feel. CGMs can be off by 15-20%, especially during rapid sugar changes. Always treat symptoms, not just numbers. If you feel low, check with a meter.
What happens if my pump breaks or stops working?
If your pump stops, you’re at risk for diabetic ketoacidosis (DKA) within 4 to 6 hours. Always carry backup insulin pens and syringes. If your pump fails, switch to your backup immediately. Inject your usual basal insulin dose every 2 to 3 hours, and correct highs with bolus doses. Contact your pump company for a replacement - most offer overnight shipping for emergencies. Never wait to act.
Can I swim or shower with an insulin pump?
It depends on the pump. Tubeless patch pumps like the Omnipod 5 are waterproof up to 3 meters for 30 minutes, so swimming and showering are fine. Tube-based pumps like Medtronic or Tandem are not waterproof - you must disconnect them before getting wet. Some people use waterproof cases or adhesive patches to protect tubing, but disconnecting is the safest option. Always check your pump’s manual for water resistance ratings.
Will my insurance cover an insulin pump?
In the U.S., most private insurers, Medicare, and Medicaid cover insulin pumps if you meet clinical criteria (like HbA1c above 7.5% or frequent hypoglycemia). In Australia, coverage depends on your private health insurance or the National Diabetes Services Scheme (NDSS). You’ll need a letter of medical necessity from your doctor. About 22% of patients report initial insurance denials - but appeals often succeed with proper documentation.
What to Do Next
If you’re thinking about a pump, start by talking to your diabetes care team. Ask for a referral to a certified diabetes educator who specializes in insulin pumps. Ask to meet someone who’s been using one for at least a year. Watch videos of people changing their infusion sets. Read reviews from real users - not just the manufacturer’s website.Don’t rush. This isn’t a gadget. It’s a medical device that requires commitment. But if you’re ready to take control, it can give you back hours of your day - and peace of mind you didn’t know you were missing.


Comments
Sabrina Thurn
December 9, 2025 AT 22:05Insulin pump therapy is a game-changer for people with high variability in glucose levels. The ability to fine-tune basal rates down to 0.01 units makes a huge difference in overnight stability. I’ve seen patients go from HbA1c 9.8% to 7.1% in six months just by switching to a hybrid closed-loop system. The tech isn’t perfect, but the precision is unmatched.
Just remember: it’s not a set-and-forget device. You still need to carb count, monitor trends, and carry backup. But the freedom? Worth every beep and alarm.
Also, the Omnipod 5’s tubeless design is a lifesaver for active folks-no more tubing snagging on door handles during a sprint to catch the bus.
Asset Finance Komrade
December 10, 2025 AT 17:41Let’s be honest: this reads like a corporate whitepaper disguised as a patient guide. 🤖
Yes, pumps reduce nocturnal hypoglycemia. So do sleeping with a spouse who wakes you up when you’re sweating. And yes, they cost $5k. So does a new iPhone. But we’re told this is ‘medical necessity’ while rent goes up 15% a year.
It’s not the tech that’s the problem-it’s the system that makes it a luxury. I’d rather have universal healthcare than a smarter pump.
Jennifer Blandford
December 11, 2025 AT 03:42OMG I JUST SWITCHED TO OMNIPOD 5 LAST MONTH AND I’M CRYING RIGHT NOW 😭
My 7-year-old used to wake up screaming from lows at 3am. Now? We sleep. Like, actual sleep. No more midnight glucose checks. No more panic. I didn’t think it was possible to feel this… normal again.
Yes, the pump beeps. Yes, I still carry pens. Yes, I freaked out when it fell off in the pool. But this? This is freedom. Thank you to everyone who made this tech real.
Also, my kid now calls it her ‘robot insulin dragon’ and it’s the cutest thing ever.
Brianna Black
December 11, 2025 AT 22:39As someone who has managed Type 1 for over 22 years, I can say with absolute certainty that insulin pump therapy has transformed my quality of life. The shift from MDI to hybrid closed-loop was not just clinical-it was existential.
Before, I lived in fear of the next low. Now, I plan dinners, travel, and weekend hikes without a spreadsheet. The data from my CGM and pump is a conversation with my body, not a battle.
And yes, the cost is absurd. But when you consider the lifetime savings on diabetic complications-retinopathy, neuropathy, dialysis-the investment pays for itself. Insurance denials are a scandal, not a policy.
For anyone considering it: do the research. Talk to users. Don’t let fear of tech override the chance at real stability.
Shubham Mathur
December 13, 2025 AT 03:56People talk about pumps like they’re magic but they forget one thing-your body still has to work with it. I had a guy at work who switched to pump and then ignored all the alarms because he was ‘too busy’. He ended up in the ER with DKA. You think your phone dying is bad? Try running out of insulin for 6 hours.
And the skin irritation? I’ve seen people with sores on their stomachs from the adhesive. It’s not just ‘mild redness’-it’s chemical burns in some cases.
Also, why do all these devices assume you have perfect vision? The screens are tiny, the menus are confusing, and if you’re tired? Good luck. This isn’t user-friendly-it’s user-exploitative.
And don’t get me started on the cost. $5000 for a plastic box? In India, we use syringes and still live. This feels like corporate greed wrapped in medical jargon.
Stacy Tolbert
December 13, 2025 AT 11:58I used to love my pump. Then I got a bad infection at the site and spent three weeks in pain. Then the tubing kinked during a date and I had to stop at a gas station to fix it while my partner waited in the car. Then the alarm went off at 4am for a ‘sensor error’ and I screamed into my pillow.
Now I’m back on injections. And I’m not mad. I’m just… tired. The tech promised freedom but delivered more stress. I just want to be left alone to manage my diabetes without a device that judges me every 15 minutes.
Ronald Ezamaru
December 13, 2025 AT 13:04One thing no one talks about enough: the emotional labor of managing a pump. It’s not just the tech-it’s the constant vigilance. You’re not just a person with diabetes anymore. You’re a system administrator for your own body.
That’s heavy. And it’s not something you can just ‘get used to’. It changes how you think about food, sleep, stress, even relationships.
Some people thrive. Others burn out. And the system doesn’t give enough space for the latter.
There’s no shame in choosing injections. It’s not failure. It’s adaptation.
Ryan Brady
December 14, 2025 AT 11:35Why are we even talking about this? In America, we’re supposed to fix problems, not buy $7000 gadgets to cope with them. This is what happens when healthcare is a profit center. You get a fancy pump instead of affordable insulin. You get tech instead of justice.
And don’t get me started on how they market this to parents like it’s a Christmas present. ‘Your kid can finally be normal!’ No. Your kid can finally be a tech support ticket.
Just give us cheap insulin and stop selling us snake oil wrapped in Bluetooth.
Raja Herbal
December 16, 2025 AT 10:58Oh wow, so now we’re glorifying medical devices as if they’re smartphones? 😏
Let me guess-you also think your Fitbit is a therapist? You don’t need a pump to control your sugar. You need discipline. You need to eat less sugar. You need to stop blaming your body for your choices.
My cousin in Delhi uses syringes, works two jobs, and has an HbA1c of 6.9. No pump. No alarms. Just willpower.
Stop making diabetes a tech problem. It’s a lifestyle problem. And you’re all just buying into the corporate lie.
Michael Robinson
December 18, 2025 AT 05:06It’s not about the machine. It’s about the person behind it.
Some people need the pump. Some don’t. Neither is better. Neither is worse.
It’s just what works for you.
Don’t let anyone make you feel like you’re not trying hard enough because you use a needle. Or because you use a pump.
You’re doing the best you can. That’s enough.
Kathy Haverly
December 18, 2025 AT 17:03Let’s not pretend this is about health. It’s about market expansion. The pump industry spends more on marketing than on R&D. They target kids because parents are emotionally vulnerable. They use ‘freedom’ as a buzzword to sell dependency.
And don’t even get me started on the data harvesting. Your glucose trends, your eating habits, your sleep patterns-your body is now a product.
It’s not innovation. It’s surveillance with a side of insulin.
Evelyn Pastrana
December 20, 2025 AT 16:01My mom switched to a pump after 30 years of injections. She said, ‘I finally feel like I’m living, not managing.’
And then she cried for an hour because she realized she’d spent decades being afraid to eat pizza.
That’s the real win.
Not the tech.
The pizza.
Nikhil Pattni
December 21, 2025 AT 11:06Look I’ve been using Omnipod 5 for 14 months now and I can tell you the truth it’s not perfect but it’s the best thing that happened to me since I got diagnosed at 19 I used to have 5-6 lows a week now it’s maybe one a month and I actually go out with friends without checking my glucose every 20 minutes I even went to a concert last weekend and didn’t panic once and yes I carry backup pens and yes I still have to check my sugar but the freedom to just live is worth every single alarm and every single time I’ve had to replace a pod because it fell off in the shower I mean honestly if you’re scared of tech you’re scared of life because diabetes doesn’t care if you’re scared it’s always there and the pump doesn’t make it go away it just gives you the tools to not let it own you so if you’re on the fence just talk to someone who’s been there for a year and stop listening to the fear porn on Reddit because most of it’s just people who don’t understand the difference between a tool and a crutch and also I just want to say thank you to the engineers who made this possible because I’m not a robot but sometimes I feel like one and that’s okay
Arun Kumar Raut
December 23, 2025 AT 09:46For anyone thinking about a pump: start small. Borrow one from your clinic. Try it for a week. See how you feel.
Don’t rush. Don’t compare yourself to others. Some people thrive with tech. Others need simplicity. Both are valid.
And if you’re a parent? Talk to your kid-not just the doctor. What do they want? What scares them?
This isn’t just medicine. It’s a life decision.
And you’ve got this.