Every year, tens of thousands of people end up in the emergency room because they took too much of a common pain reliever-one they thought was completely safe. Acetaminophen, the active ingredient in Tylenol and hundreds of other OTC products, is the leading cause of acute liver failure in the United States. It’s in your cold medicine, your sleep aid, your headache tablet, and even your prescription painkiller. And most people have no idea they’re at risk.
Why Acetaminophen Is So Dangerous
Acetaminophen works great for pain and fever. It’s gentle on the stomach, unlike NSAIDs like ibuprofen or aspirin. But here’s the catch: your liver breaks it down. At normal doses, it’s harmless. At higher doses, or when taken too often, your liver gets overwhelmed. It produces a toxic byproduct called NAPQI. Normally, your liver uses an antioxidant called glutathione to neutralize it. But if you take too much acetaminophen, glutathione runs out. Then NAPQI starts destroying liver cells. It doesn’t take much to tip the scale.
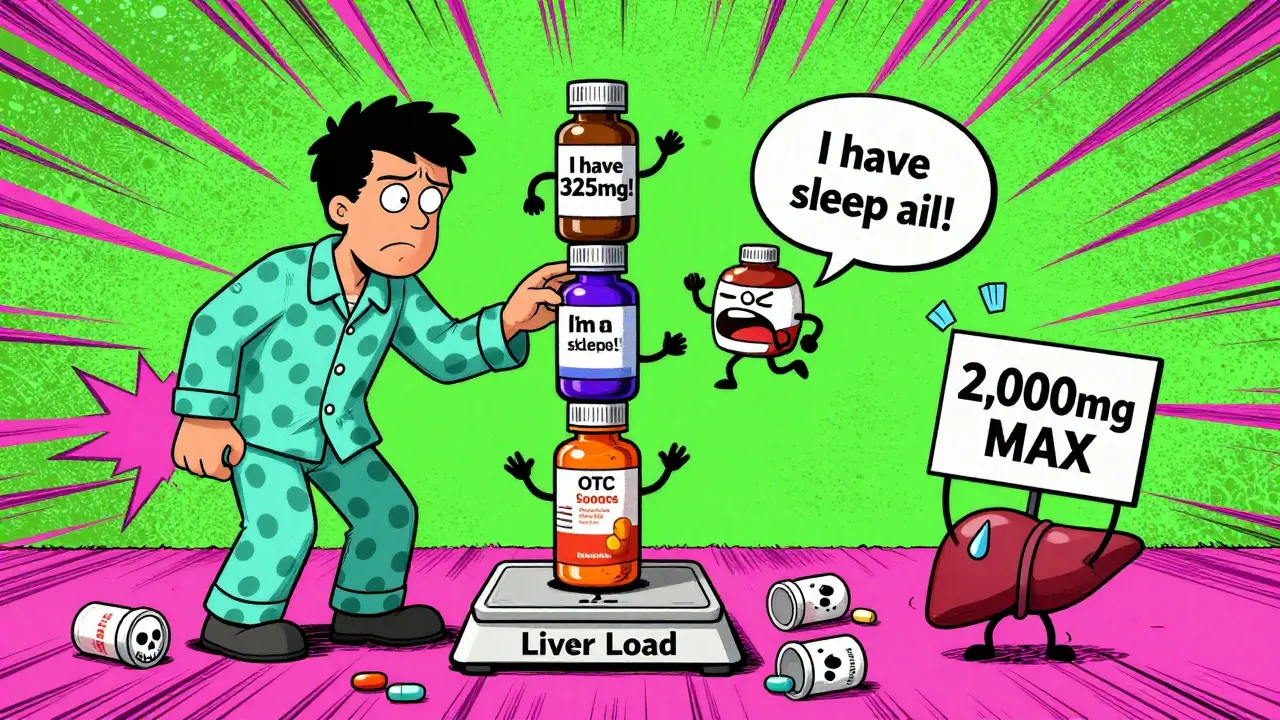
The FDA says the max daily dose for healthy adults is 4,000 mg. That sounds like a lot-until you realize how easy it is to hit that limit without meaning to. One extra-strength Tylenol tablet is 500 mg. Four of those get you to 2,000 mg. Add a cold medicine with 325 mg of acetaminophen? You’re at 2,325 mg. Now take another Tylenol at bedtime? You’re over 2,800 mg. Do that for three days straight? You’re in danger zone.
The Hidden Danger: Combination Products
More than half of unintentional overdoses happen because people don’t realize they’re taking acetaminophen more than once. Cold and flu meds? They’ve got it. Sleep aids? Often have it. Prescription painkillers like Vicodin or Percocet? Always have it. A 2022 FDA review found that 25% of accidental overdoses came from people taking multiple products without checking the labels.
There are over 600 OTC and prescription medications that contain acetaminophen. If you’re not reading every label, you’re playing Russian roulette with your liver. That cough syrup you took last night? Might have had 160 mg. The headache pill you took this morning? Another 500 mg. You think you’re being careful. You’re not.
Who’s at Highest Risk?
You might think only heavy drinkers are at risk. Not true. People with fatty liver disease, hepatitis, or even just a history of heavy alcohol use are more vulnerable. But even healthy people can overdose if they take too much over several days.
If you have liver disease-whether it’s from alcohol, hepatitis B or C, or NAFLD-the rules change. The Veterans Affairs Hepatitis Resource Center recommends no more than 2,000 mg per day. Some experts say 1,500 mg is safer. And if you drink alcohol? Cut it to 1,000 mg per day-or avoid acetaminophen entirely. Alcohol and acetaminophen together are a deadly combo. They slash your liver’s ability to detoxify the drug, making a toxic dose much lower than you’d expect.
NSAIDs Aren’t the Safe Alternative
People often switch to ibuprofen or naproxen thinking they’re safer for the liver. But that’s a myth. While NSAIDs don’t cause liver damage as often as acetaminophen, they’re not harmless. Diclofenac, in particular, is linked to rare but serious liver injury. More importantly, NSAIDs can wreck your kidneys, cause stomach bleeding, and raise blood pressure. If you have liver disease, you’re already at higher risk for kidney problems. NSAIDs make that worse.
For people with cirrhosis or advanced liver disease, the University Hospitals 2023 guidelines say: avoid NSAIDs. They can trigger dangerous fluid buildup and worsen kidney function. So switching from acetaminophen to ibuprofen doesn’t solve the problem-it just swaps one risk for another.
How to Use OTC Pain Relievers Safely
- Read every label. Look for “acetaminophen,” “APAP,” or “paracetamol.” If you see it, don’t take anything else with it.
- Never exceed 3,000 mg per day. Even if the label says 4,000 mg, aim lower. Your liver doesn’t need the extra stress.
- Wait at least 8 hours between doses. Don’t take a pill every 4 hours just because you can. Your liver needs time to process it.
- Avoid alcohol completely. No matter how small the dose, mixing it with acetaminophen increases liver damage risk.
- Use a pill organizer. Mark each slot with the max daily limit. If you’ve already taken your 3,000 mg by noon, stop.
- Keep a medication diary. Write down every pill you take, including cold medicine, sleep aids, and prescriptions. Review it weekly.
What Are the Warning Signs?
Liver injury doesn’t always come with a siren. It creeps up. You might feel fine until you suddenly feel awful. The National Institute of Diabetes and Digestive and Kidney Diseases says 93% of acetaminophen-induced liver failure cases show these symptoms within 24 to 72 hours:
- Nausea or vomiting
- Loss of appetite
- Fatigue or weakness
- Pain in the upper right side of your belly
- Dark urine
- Clay-colored stools
- Yellowing of the skin or eyes (jaundice)
If you’ve taken acetaminophen in the last 24 hours and you have even one of these symptoms, go to the ER. Don’t wait. Don’t call your doctor tomorrow. Go now. The antidote, N-acetylcysteine (NAC), works best if given within 8 hours of overdose. After 16 hours, its effectiveness drops sharply.

Alternatives for Chronic Pain
If you’re on daily pain medication because of arthritis, back pain, or another condition, there are better long-term options than relying on pills.
- Topical pain relievers. Gels and patches with NSAIDs (like diclofenac gel) deliver the drug straight to the skin. Very little gets into your bloodstream. That means less stress on your liver.
- Physical therapy. Strengthening muscles around sore joints reduces pain naturally. Studies show it works as well as pills for many people.
- Cognitive behavioral therapy (CBT). Chronic pain isn’t just physical-it’s mental. CBT helps you change how you respond to pain. The American Liver Foundation says it’s one of the best first-line treatments.
- Acupuncture. Multiple studies show it reduces pain in people with osteoarthritis and back pain. No drugs. No side effects.
The NIH is spending $47 million over the next few years to develop painkillers that don’t go through the liver. But until then, the safest strategy is to use the lowest effective dose for the shortest time possible.
What About Genetic Testing?
Some people have a genetic variation that makes them break down acetaminophen slower. Companies like 23andMe now offer tests that can identify these variations. If you’ve had unexplained liver issues or you’re on long-term pain meds, a genetic test might help you understand your personal risk. It’s not for everyone-but if you’re high-risk, it’s worth asking your doctor about.
Final Rule: When in Doubt, Skip It
You don’t need to take pain relievers every day. Sometimes rest, ice, heat, or stretching works better. If you’re taking acetaminophen more than three days a week for more than a few weeks, talk to your doctor. There’s almost always a better way.
Acetaminophen isn’t evil. It’s just powerful. And like any powerful tool, it needs respect. A single extra-strength tablet might seem harmless. But stacked up over days, it can destroy your liver without warning. Know your dose. Read your labels. Protect your liver. Your future self will thank you.
Can I take acetaminophen if I have a fatty liver?
Yes-but only if you keep your daily dose under 2,000 mg. Fatty liver disease reduces your liver’s ability to detoxify drugs, so the safe limit drops. Avoid alcohol completely. Talk to your doctor before using it long-term.
Is it safe to take Tylenol with ibuprofen?
It can be, but only if you stay under the daily limits for both. Don’t combine them for more than a few days. Use the lowest effective dose of each. For example: 500 mg acetaminophen every 6 hours (max 2,000 mg/day) and 200 mg ibuprofen every 8 hours (max 600 mg/day). Never exceed either limit.
Why do cold medicines contain acetaminophen?
Because it’s effective at reducing fever and mild pain, which are common cold symptoms. But manufacturers assume people will only take one product at a time. Most don’t realize they’re doubling up. That’s why the FDA now requires clear labeling and “liver warning” icons on the front.
What if I accidentally took too much acetaminophen?
Call Poison Control immediately (1-800-222-1222 in the U.S.) or go to the ER. Don’t wait for symptoms. Even if you feel fine, liver damage can start without warning. The antidote NAC works best if given within 8 hours.
Are there OTC pain relievers that are completely safe for the liver?
No OTC painkiller is 100% safe-but topical NSAIDs (like diclofenac gel) come closest. They deliver pain relief with almost no liver exposure. For mild pain, try heat, cold, or stretching. For chronic pain, consider physical therapy or acupuncture before reaching for pills.

