Understanding Hepatic Encephalopathy
Hepatic encephalopathy (HE) is a serious and complex neurological complication that arises from liver dysfunction. It is characterized by a wide range of neuropsychiatric symptoms, including confusion, disorientation, and even coma. The severity of these symptoms is often linked to the degree of liver damage present.
As a blogger, my goal is to help you better understand this condition and learn how liver transplantation plays a crucial role in its treatment. In this article, I will delve into the various aspects of hepatic encephalopathy and how a liver transplant can provide relief from its symptoms.
The Liver's Role in Preventing Hepatic Encephalopathy
The liver is an essential organ that performs numerous vital functions, including detoxification, metabolism, and protein synthesis. One of its primary roles is to filter out toxins and waste products from the bloodstream, ensuring they do not build up and cause harm to the body.
In the case of hepatic encephalopathy, the liver is unable to effectively remove these toxins, particularly ammonia, which can accumulate in the brain and cause neurological symptoms. The liver's reduced ability to perform its detoxification function is a critical factor in the development of hepatic encephalopathy, making it essential to address any underlying liver issues for successful treatment.
Causes and Risk Factors of Hepatic Encephalopathy
There are several factors that contribute to the development of hepatic encephalopathy. The most common cause is cirrhosis, a chronic liver disease that results from long-term damage to the liver, often due to alcohol abuse or viral hepatitis. Other factors that can increase the risk of developing hepatic encephalopathy include:
- Liver cancer
- Portal hypertension
- Congenital liver abnormalities
- Infections
- Certain medications that suppress liver function
It is essential to identify and address any underlying causes of hepatic encephalopathy to effectively manage the condition and prevent further liver damage.
Recognizing the Symptoms of Hepatic Encephalopathy
Hepatic encephalopathy can manifest in various symptoms, ranging from mild cognitive disturbances to severe neurological impairment. These symptoms often worsen with the progression of liver disease. Some common symptoms of hepatic encephalopathy include:
- Confusion and disorientation
- Mental sluggishness
- Memory problems
- Personality changes
- Sleep disturbances
- Muscle tremors and weakness
- Seizures
- Coma
Early detection and intervention are crucial in managing hepatic encephalopathy and preventing further complications.
Diagnosing Hepatic Encephalopathy
Diagnosing hepatic encephalopathy can be challenging due to the varied nature of its symptoms. A thorough medical evaluation, including a detailed patient history and physical examination, is necessary to identify any underlying liver disease and rule out other potential causes of the symptoms. Blood tests, imaging studies, and, in some cases, a liver biopsy may be required to confirm the diagnosis and assess the extent of liver damage.
Conventional Treatment Options for Hepatic Encephalopathy
Once hepatic encephalopathy is diagnosed, the primary focus of treatment is to address the underlying liver dysfunction and manage the neurological symptoms. Conventional treatment options include:
- Medications to reduce ammonia levels in the blood
- Antibiotics to treat infections
- Lactulose, a laxative that helps eliminate toxins from the body
- Dietary modifications to reduce protein intake and manage ammonia levels
- Treatment of any underlying liver diseases, such as cirrhosis or hepatitis
While these treatments can help manage the symptoms of hepatic encephalopathy, they often do not provide a long-term solution, especially in cases of severe liver damage.
Liver Transplantation as a Treatment for Hepatic Encephalopathy
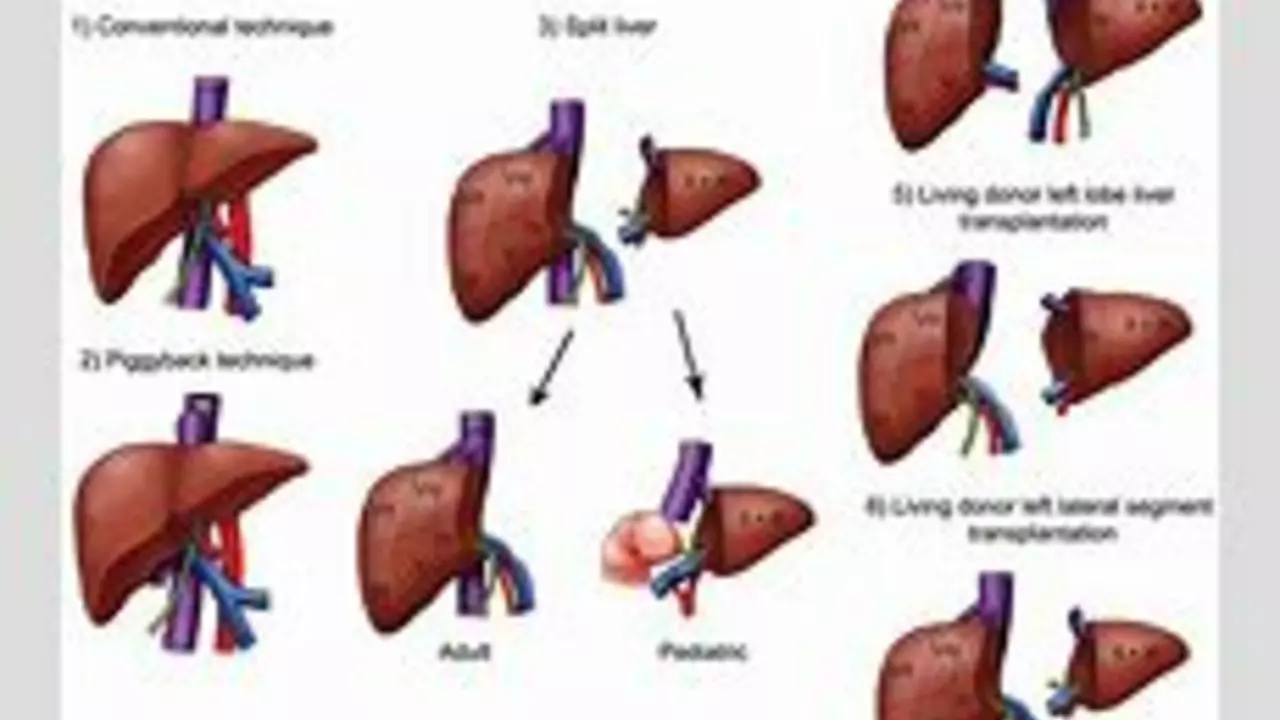
In cases where hepatic encephalopathy is caused by severe liver damage or cirrhosis, a liver transplant may be the only viable treatment option. A liver transplant involves replacing the damaged liver with a healthy one from a deceased or living donor. Liver transplantation has been shown to significantly improve survival and quality of life in patients with hepatic encephalopathy, often leading to complete resolution of neurological symptoms.
However, liver transplantation is a major surgery with potential risks and complications, and not all patients may be eligible for the procedure. Factors such as age, overall health, and the availability of a suitable donor can impact the likelihood of a successful liver transplant.
Post-Transplant Care and Recovery
After a liver transplant, patients must undergo careful monitoring and follow a strict post-transplant care regimen to ensure the success of the procedure and prevent complications. This may include lifelong immunosuppressive medications to prevent organ rejection, regular blood tests and imaging studies to monitor liver function, and ongoing management of any underlying medical conditions.
Patients must also make certain lifestyle modifications, such as avoiding alcohol, following a healthy diet, and exercising regularly to promote overall health and maintain optimal liver function.
The Importance of Early Intervention and Comprehensive Care
Hepatic encephalopathy is a complex and potentially life-threatening condition that requires prompt diagnosis and comprehensive care. Early intervention, appropriate management of underlying liver disease, and consideration of liver transplantation as a treatment option are critical to improving outcomes and enhancing the quality of life for patients with hepatic encephalopathy.
As a blogger, my hope is that this article has provided valuable insights into the role of liver transplantation in the treatment of hepatic encephalopathy and underscored the importance of a holistic approach to managing this challenging condition.

Comments
mas aly
June 26, 2023 AT 05:43Hepatic encephalopathy often stems from an accumulation of ammonia produced by gut bacteria, and while lactulose helps trap it in the colon, newer probiotics are showing promise in modulating that microbial load. Recent studies suggest that a diet rich in fiber can reduce systemic ammonia levels by encouraging beneficial bacterial growth. It's also worth noting that early detection of subtle cognitive changes can shift treatment timelines dramatically. Keeping an eye on subtle shifts in attention or short‑term memory can make a big difference before severe episodes develop. Overall, integrating dietary measures with standard pharmacotherapy creates a more holistic approach.
Abhishek Vora
June 29, 2023 AT 09:57The literature unequivocally demonstrates that approximately 30–40 % of cirrhotic patients will experience at least one overt episode of hepatic encephalopathy during their disease course. Moreover, the mortality risk escalates sharply once neurological symptoms become overt, underscoring the urgency of timely intervention. While lactulose remains a cornerstone, rifaximin has emerged as a potent adjunct, reducing recurrence rates by nearly half in controlled trials. Consequently, clinicians must adopt a multitiered strategy rather than rely on a single therapeutic avenue.
maurice screti
July 2, 2023 AT 14:11When one delves into the intricate pathophysiology of hepatic encephalopathy, the narrative unfolds like a meticulously crafted novel, each chapter revealing a new layer of complexity that demands both scientific rigor and compassionate insight. The liver, as the body's chief detoxifier, employs an elegant cascade of enzymatic reactions to convert neurotoxic ammonia into urea, a harmless molecule destined for renal excretion. Yet, in the setting of cirrhosis, this delicate balance is thrown asunder, allowing ammonia and a host of other gut‑derived metabolites to seep across the blood‑brain barrier. This breach precipitates astrocyte swelling, altered neurotransmission, and ultimately the bewildering cognitive dysfunction that patients describe as “brain fog.” Adding to this tapestry are inflammatory cytokines, whose surges further exacerbate neuronal excitability and compromise synaptic integrity. It is no surprise, then, that clinicians have turned to a multimodal therapeutic armamentarium, combining lactulose’s osmotic effect with rifaximin’s antimicrobial precision. The former sequesters ammonia within the colon, while the latter trims the bacterial populations that generate it, creating a synergistic reduction in systemic toxin load. Moreover, recent forays into fecal microbiota transplantation have opened a frontier where the gut’s ecological balance can be restored in a more holistic fashion, potentially offering lasting remission where conventional treatments falter. The specter of liver transplantation looms large as the definitive resolution for those whose hepatic architecture has deteriorated beyond repair; however, the scarcity of suitable donor organs renders this option an aspirational, not an immediate, remedy for many. Post‑transplant, patients must navigate the treacherous waters of immunosuppression, vigilance against rejection, and lifestyle modifications that can feel as daunting as the disease itself. Nonetheless, the survival benefits and quality‑of‑life improvements reported in longitudinal cohorts unequivocally attest to the procedure’s transformative power. In parallel, the medical community continues to refine prognostic scoring systems, such as the Model for End‑Stage Liver Disease (MELD) and the West Haven criteria, to better stratify risk and prioritize transplant candidacy. Education, too, plays a pivotal role: patients and caregivers who recognize early neurocognitive shifts can seek intervention before irreversible damage ensues. Ultimately, the journey from hepatic dysfunction to encephalopathic manifestation underscores a profound interplay between organ systems, microbial ecosystems, and therapeutic ingenuity, reminding us that medicine is as much an art of integration as it is a science of precision.
Abigail Adams
July 5, 2023 AT 18:25It is lamentable how often the discourse surrounding hepatic encephalopathy reduces the patient to a mere biochemical anomaly, neglecting the profound psychosocial ramifications that accompany cognitive decline. While the clinical guidelines enumerate pharmacologic regimens with commendable clarity, they fall short in addressing the stigma that patients endure when their mental faculties waver. A holistic approach must therefore encompass not only transplant eligibility but also robust psychological support networks. Without such comprehensive care, the therapeutic gains risk being undermined by isolation and despair.
Belle Koschier
July 8, 2023 AT 22:39Balancing the urgency of transplant with the realities of donor availability is a delicate dance, and I appreciate how the article underscores both sides of the equation. At the same time, integrating lifestyle counseling early on can empower patients to manage symptoms while awaiting surgery. A multidisciplinary team-hepatologists, nutritionists, and neuropsychologists-offers the most compassionate pathway forward.
Allison Song
July 12, 2023 AT 02:53Indeed, the interplay between gut microbiota and ammonia production is a fascinating frontier that bridges hepatology and neurobiology. Philosophically, one might argue that the body’s internal ecosystems reflect a microcosm of broader ecological principles, wherein balance begets health. Recognizing this, clinicians could consider microbiome‑targeted therapies as adjuncts rather than mere afterthoughts. In this light, the patient’s journey becomes a collaborative negotiation with their own biology.
Joseph Bowman
July 15, 2023 AT 07:07One can’t help but wonder whether the allocation committees are truly transparent, or if hidden agendas sway the decision matrix for transplant candidacy. While the medical criteria appear objective, subtle biases-perhaps economic or political-can creep into the final call. This conspiratorial undercurrent, whether real or perceived, underscores the need for vigilant oversight.
Singh Bhinder
July 18, 2023 AT 11:22The diagnostic process can feel like searching for a needle in a haystack, especially when early cognitive signs masquerade as fatigue or depression. A thorough neuropsychological battery, paired with ammonia profiling, can sharpen the diagnostic lens. Early identification not only improves outcomes but also reduces the emotional toll on families.
Kelly Diglio
July 21, 2023 AT 15:36I appreciate the depth of the previous exposition, particularly the emphasis on emerging therapies such as fecal microbiota transplantation. While still experimental, these approaches underscore the importance of addressing the gut‑brain axis holistically. It also highlights the need for more rigorous clinical trials to validate efficacy. Until then, clinicians should remain open-minded yet cautious when integrating novel modalities.
Carmelita Smith
July 24, 2023 AT 19:50Transplant remains the only definitive cure for advanced hepatic encephalopathy. 😊
Liam Davis
July 28, 2023 AT 00:04Patients undergoing liver transplantation must adhere to a stringent post‑operative regimen: immunosuppressants to prevent rejection, regular imaging to monitor graft function, and lifelong dietary modifications to sustain liver health. Moreover, the psychological adjustment cannot be overstated; many individuals experience anxiety about graft viability and fear of relapse. Support groups, both in‑person and virtual, provide a vital forum for sharing experiences and coping strategies. Importantly, adherence to medication schedules has been correlated with improved survival rates, underscoring the necessity of structured routines. Healthcare providers should also educate patients on recognizing early signs of infection, given their heightened susceptibility under immunosuppression. Finally, regular follow‑ups with a multidisciplinary team ensure that any complications are addressed promptly, enhancing overall quality of life.
Arlene January
July 31, 2023 AT 04:18Hey, just wanted to say that anyone dealing with this condition deserves massive credit for hanging in there – it’s a tough ride! Keep pushing, and remember that every small improvement is a win.
Kaitlyn Duran
August 3, 2023 AT 08:32When my uncle was diagnosed with hepatic encephalopathy, the whole family felt like we were in a fog ourselves, trying to understand medical jargon while caring for him. It helped immensely when the care team broke things down into plain language and involved us in the decision‑making process. That collaborative vibe made the whole transplant journey feel less intimidating.
Terri DeLuca-MacMahon
August 6, 2023 AT 12:46Great rundown! 👏 Post‑transplant care really is a marathon, not a sprint, and those support networks can make all the difference. Keep sharing this info! 🌟
gary kennemer
August 9, 2023 AT 17:00From a philosophical standpoint, the notion of “balance” you mentioned resonates with the concept of homeostasis as a dynamic equilibrium-an ever‑adjusting state rather than a static condition. This perspective invites clinicians to view interventions as nudges rather than absolute fixes, fostering a more adaptable therapeutic mindset. Such a view also aligns with patient‑centered care, where flexibility accommodates individual variations in disease progression.
Payton Haynes
August 12, 2023 AT 21:15The pharmaceutical industry certainly has a stake in keeping patients on chronic medication regimens, which can be lucrative. It’s worth questioning whether newer, potentially cheaper alternatives receive the same push for adoption. Transparency in drug pricing could help patients make more informed choices.
Earlene Kalman
August 16, 2023 AT 01:29This article is overly optimistic; transplant isn’t a magic bullet for everyone.
Brian Skehan
August 19, 2023 AT 05:43While the benefits of transplantation are clear, we must stay vigilant about the hidden costs-both financial and physiological-that can lurk beneath the surface of successful outcomes.