Guillain-Barré Syndrome (GBS) doesn’t start with a bang. It creeps in quietly-maybe a tingling in your toes, a stumble on the stairs, or legs that feel heavier than usual. Within days, that mild discomfort can turn into full-body weakness, paralysis, and even the inability to breathe. It’s rare, affecting only 1 to 2 people per 100,000 each year, but when it hits, it moves fast. And the clock starts ticking the moment symptoms appear.
What Happens When Your Immune System Turns Against You
GBS is an autoimmune disorder. Your body’s own immune system, which normally fights off viruses and bacteria, mistakenly attacks the protective covering around your peripheral nerves-the myelin sheath. This slows down or blocks nerve signals, leading to muscle weakness that starts in the feet and legs and moves upward. In 85% of cases, it climbs from the lower body to the arms, face, and even the muscles that control breathing. The most common form, called Acute Inflammatory Demyelinating Polyradiculoneuropathy (AIDP), makes up 90% of cases in North America and Europe. Doctors confirm this through nerve conduction tests that show slowed signals. Another version, axonal GBS, damages the nerve fibers themselves and is more common after infections like Zika or Campylobacter jejuni, which triggers about 20 to 40% of cases in the U.S. after a bad stomach bug. You won’t always know what caused it. But infections are the usual suspects: Campylobacter, cytomegalovirus, Epstein-Barr, and even the flu. In rare cases, surgery or vaccines have been linked. The key is timing-symptoms usually show up 1 to 4 weeks after the infection clears.Why This Is a Medical Emergency
GBS isn’t something you can wait out at home. About 20 to 30% of patients end up on a ventilator because the muscles that control breathing fail. That can happen within just 7 days of the first symptoms. That’s why hospitalization is required the moment GBS is suspected. Other dangers include unstable blood pressure, irregular heart rhythms, and trouble swallowing-all signs of autonomic nervous system failure. These affect 65% of severe cases. Continuous heart and blood pressure monitoring is standard. If you can’t walk, can’t lift your head, or can’t take a deep breath, you need intensive care. Doctors use specific criteria to diagnose GBS: progressive weakness in more than one limb, loss of reflexes, and typical nerve test results. A spinal tap often shows high protein levels with normal cell counts-a sign called albuminocytological dissociation. That’s a key clue that helps rule out mimics like botulism or myasthenia gravis, which get misdiagnosed in up to 10% of cases.IVIG: The First-Line Treatment That Saves Lives
The two main treatments for GBS are intravenous immunoglobulin (IVIG) and plasma exchange. Both work by calming the overactive immune system. But IVIG is now the go-to choice in most hospitals. IVIG is made from donated human blood plasma packed with antibodies. When given in high doses-0.4 grams per kilogram of body weight daily for five days-it essentially distracts the immune system. Instead of attacking nerves, it targets the foreign antibodies in the IVIG bag. Studies show IVIG cuts recovery time by about half. Patients who get it within two weeks of symptoms start walking independently three weeks sooner than those who don’t. Sixty percent show improvement within 2 to 4 weeks, compared to just 40% in untreated groups. That’s not just a small benefit-it’s life-changing. It’s also easier. IVIG just needs a standard IV line. Plasma exchange requires a central line, filtering your blood through a machine over several sessions. That’s more invasive, more risky, and takes longer. Patients report better comfort scores with IVIG, even though both treatments lead to similar functional outcomes at four weeks.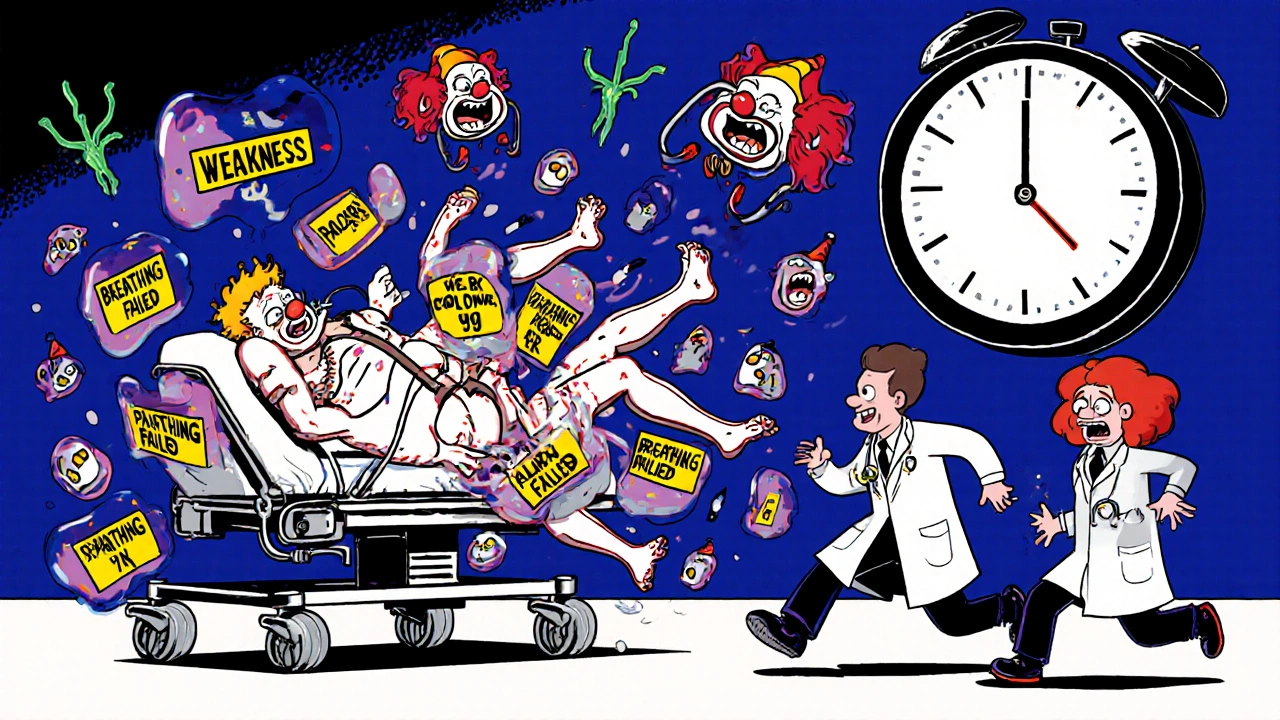
Cost, Side Effects, and When IVIG Isn’t an Option
IVIG isn’t cheap. A full course in the U.S. costs between $15,000 and $25,000. Plasma exchange runs a bit higher, around $20,000 to $30,000. But because IVIG is simpler to give, most hospitals choose it first. Side effects are common but usually manageable. Headaches hit about 25% of patients-some describe them like a vice squeezing their skull. Fever, chills, and nausea happen in 15%. More serious risks include blood clots (1-3%) and kidney problems, especially in people with pre-existing conditions. One case report noted acute renal failure after the third dose, requiring dialysis. That’s rare-under 0.5%-but it happens. IVIG is dangerous for people with IgA deficiency. Their bodies can react violently to the antibodies in the treatment, triggering anaphylaxis. In those cases, plasma exchange is the only safe option. And there’s another problem: supply. During the 2020-2022 pandemic, global shortages affected 40% of hospitals. If you live in a rural area or your hospital’s supply runs low, getting IVIG on time can be a struggle.What Doesn’t Work-And Why
Corticosteroids like prednisone were once thought to help. But after multiple large trials, the data is clear: steroids don’t speed up recovery. A 2017 Cochrane review found no difference between steroid users and placebo groups. That’s why they’re not recommended. The same goes for antibiotics, antivirals, or herbal supplements. GBS isn’t caused by an active infection you can kill off-it’s an immune mistake. Treating the original bug won’t stop the attack on your nerves.
Recovery: The Long Road Back
Recovery doesn’t end when you leave the hospital. It takes months. About 60% of people recover fully within 6 to 12 months. Another 30% have lingering weakness-maybe trouble climbing stairs, gripping objects, or walking without a cane. Around 10% remain severely disabled after a year. Patient stories tell the real story. One person on a GBS forum said, “By day 12 of IVIG, I could wiggle my toes. Day 18, I stood with help.” Another wrote, “The headaches during the infusion were brutal.” Physical therapy is critical. Even when you’re weak, movement prevents muscle atrophy and joint stiffness. Occupational therapy helps with daily tasks. And mental health support? Essential. Depression and anxiety are common during recovery.What’s Next? Research on the Horizon
Scientists are working on better treatments. One promising drug, eculizumab, blocks part of the immune system’s attack on nerves. A 2022 trial showed patients recovered 30% faster than with IVIG alone. It’s not approved yet, but phase 3 trials are underway. Researchers are also looking at biomarkers. If you have certain anti-ganglioside antibodies in your blood, you might respond better to one treatment over another. That could lead to personalized therapy-tailoring treatment based on your immune profile. The International GBS Outcome Study (IGOS), tracking 1,500 patients across 30 countries, is testing whether starting IVIG within 72 hours of symptoms improves long-term outcomes. Early data suggests it might boost recovery by 15%.What You Need to Know Right Now
If you or someone you know suddenly develops weakness that moves upward-from feet to legs to arms-and you’ve had a recent infection, don’t wait. Go to the ER. Time matters. Every hour counts. IVIG isn’t perfect. It’s expensive, it has side effects, and supply can be spotty. But it’s the best tool we have right now. And for most people, it means the difference between months in a hospital and getting back to life. GBS doesn’t have a cure yet. But with fast diagnosis and timely IVIG, most people walk away-not just alive, but with their lives intact.What are the first signs of Guillain-Barré Syndrome?
The earliest signs are usually tingling or numbness in the feet and legs, followed by progressive weakness that moves upward. Many people notice difficulty walking, climbing stairs, or standing on their toes. Reflexes like the knee-jerk reaction often disappear. Facial weakness, trouble swallowing, or double vision can also appear early in about half of cases.
How quickly does GBS progress?
GBS typically worsens over days to weeks. Most people reach their worst point-maximum weakness-within 3 to 4 weeks after symptoms begin. In severe cases, paralysis can develop within 24 to 48 hours. If breathing becomes difficult or you can’t move your limbs, it’s an emergency.
Is IVIG the only treatment for GBS?
No, plasma exchange is also a first-line treatment and works just as well in improving recovery. But IVIG is preferred because it’s less invasive, easier to administer, and has fewer complications. Plasma exchange requires a central line and blood filtration over multiple sessions, making it harder to deliver in many hospitals.
Can GBS come back after treatment?
Relapse after initial recovery is rare-less than 5% of cases. But some people develop a related condition called chronic inflammatory demyelinating polyneuropathy (CIDP), which causes ongoing weakness. CIDP requires long-term treatment, unlike GBS, which is usually a one-time event.
How long does it take to recover from GBS?
Recovery varies. Most people start improving within 2 to 4 weeks after IVIG. Full recovery can take 6 to 12 months. About 60% return to normal function, 30% have some lasting weakness, and 10% remain severely disabled. Physical therapy plays a huge role in maximizing recovery.
Are there any new treatments for GBS on the horizon?
Yes. A drug called eculizumab, which blocks part of the immune system’s attack on nerves, showed 30% faster recovery in early trials. Researchers are also studying antibody testing to predict who will respond best to IVIG versus plasma exchange. The goal is personalized treatment-matching the right therapy to the right patient.


Comments
Darragh McNulty
November 22, 2025 AT 00:38Elaina Cronin
November 22, 2025 AT 01:46David Cusack
November 23, 2025 AT 18:28Julia Strothers
November 25, 2025 AT 12:34Erika Sta. Maria
November 27, 2025 AT 09:36Chris Vere
November 28, 2025 AT 10:25Pravin Manani
November 30, 2025 AT 08:14Mark Kahn
December 1, 2025 AT 10:59Daisy L
December 3, 2025 AT 09:01Eliza Oakes
December 3, 2025 AT 23:22Paula Jane Butterfield
December 4, 2025 AT 03:03Willie Doherty
December 4, 2025 AT 20:22Elaina Cronin
December 5, 2025 AT 11:33