Glaucoma Visual Field Test Calculator
Visual Field Test Results Calculator
Calculate your glaucoma progression risk based on Mean Deviation (MD) and Pattern Standard Deviation (PSD) values from your visual field test.
Your Results
When your eye doctor says you need a Glaucoma a progressive optic‑nerve disease that damages retinal ganglion cells and can cause irreversible vision loss evaluation, one of the key checks will be a visual field test a series of measurements that map the sensitivity of your peripheral vision. Understanding what happens during that appointment can ease anxiety and help you track the disease over time. Knowing Glaucoma early can make a huge difference in preserving sight.
Why Visual Field Testing Matters
Glaucoma often begins in the peripheral vision, where the loss is silent. Standard eye charts focus on central acuity, so a patient may feel perfectly fine while the disease silently progresses. Visual field testing captures the full picture-literally-by measuring light perception at dozens of points across the retina. The results become a baseline that your ophthalmologist or optometrist can compare against future tests, spotting subtle declines before they become obvious in daily life.
How the Test Works
Most clinics use a device called a Humphrey Field Analyzer an automated perimeter that presents flashing lights of varying brightness at specific locations. You sit in a darkened booth, place your chin on a rest, and look straight ahead at a fixed central point. The machine flashes a light in a corner of your vision and asks you to press a button as soon as you see it. The process repeats for hundreds of points, typically lasting 5-10 minutes per eye.
Types of Visual Field Tests
While the Humphrey system (Standard Automated Perimetry) is the gold standard, other methods exist to complement or substitute it in certain situations. Below is a quick comparison:
| Test | Typical Device | Strengths | Limitations |
|---|---|---|---|
| Standard Automated Perimetry uses a white‑light stimulus and evaluates the entire field | Humphrey Field Analyzer (HFA) | Highly reliable, widely studied, can detect early loss | Requires patient cooperation, longer test time |
| Frequency Doubling Technology employs low‑spatial‑frequency gratings that double in frequency | FDT perimeter | Shorter (2‑3 min), useful for screening | Less detailed, may miss subtle defects |
| Short‑Wavelength Automated Perimetry uses blue light to target the retinal nerve fiber layer | SWAP device | Can detect early damage in patients with normal white‑on‑white tests | More affected by cataracts, longer learning curve |

Preparing for Your Appointment
- Bring a list of current medications, especially eye drops.
- Inform the clinic if you wear glasses or contacts; you’ll usually remove them for the test.
- Avoid caffeine or nicotine for at least an hour; both can affect pupil size and reaction time.
- Schedule the test at a time of day when you’re alert-morning appointments often work best.
- Tell the technician about any eye conditions (e.g., cataract) that might affect results.
During the test, you’ll be asked to press a button each time you see a light. It’s okay to guess; the software accounts for false positives and negatives. If you’re unsure, simply squeeze the button-missing a stimulus will be recorded as a missed point.
Interpreting Your Results
After the test, the device generates a visual field map with several key metrics:
- Mean Deviation (MD): a single number summarizing overall loss. A negative MD indicates reduced sensitivity.
- Pattern Standard Deviation (PSD): highlights localized defects, which are typical for glaucoma.
- Glaucoma Hemifield Test (GHT): compares the upper and lower halves of the field for asymmetry.
Your clinician will compare these numbers to the baseline you established at your first test. A consistent trend of worsening MD, rising PSD, or a ‘borderline’ GHT result may trigger a change in treatment-more aggressive eye‑drop therapy, laser trabeculoplasty, or surgery.
Common Concerns and How to Address Them
Intraocular pressure the fluid pressure inside the eye, measured with a tonometer often gets mentioned alongside visual fields. High pressure is a major risk factor, but many people with normal pressure still develop glaucoma (normal‑tension glaucoma). That’s why visual field testing is essential-even if your pressure readings look fine.
Another worry: “Will the test damage my eyes?” No. The light stimuli are safe, low‑intensity flashes that pose no risk. The only discomfort is the brief fatigue from focusing for several minutes.
If you have a cataract, results may appear worse because the cloudy lens blocks light. Your doctor may order a cataract‑adjusted analysis or repeat the test after surgery.
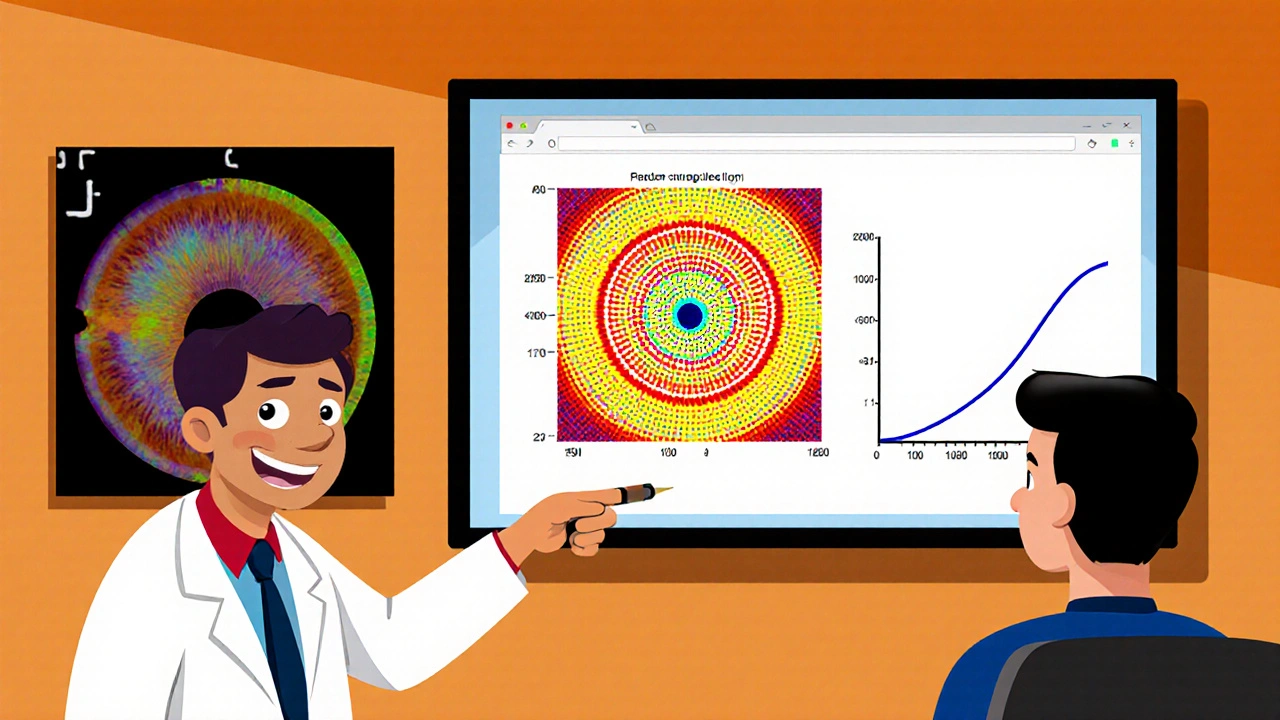
Tracking Progress Over Time
Glaucoma is a chronic condition, so regular monitoring-usually every 6-12 months-is standard. Many clinics now offer trend graphs that plot MD and PSD over years. Seeing a shallow slope can reassure you; a steep decline signals that treatment adjustments are needed.
Technology is evolving. Some practices integrate optical coherence tomography a non‑invasive imaging test that visualizes the retinal nerve fiber layer with visual field data for a more complete picture. If your provider mentions “OCT” alongside visual fields, they’re trying to correlate structural loss (seen on OCT) with functional loss (seen on the field map).
Next Steps After Your Test
- Review the printed field map with your eye‑care professional. Ask for clarification on any numbers you don’t understand.
- If treatment changes are recommended, discuss side‑effects and the expected timeline for improvement.
- Schedule your next visual field test according to the plan-most often in 6 months for newly diagnosed patients, then annually if stable.
- Maintain good eye‑health habits: regular exercise, low‑salt diet, and adherence to prescribed eye drops.
- Consider lifestyle modifications that lower systemic pressure, such as stress reduction and healthy sleep patterns; they can indirectly benefit eye pressure.
Staying informed and proactive makes the difference between maintaining a full visual field and gradually losing peripheral vision.
Frequently Asked Questions
How often should I have visual field testing?
For most glaucoma patients, an eye‑care professional recommends testing every 6 to 12 months. Frequency may increase if your disease is progressing rapidly or after a treatment change.
Is the test painful?
No. The test uses dim lights and a button press. The only discomfort is the need to remain still and focused for several minutes.
Can I take my eye drops before the test?
Yes. In fact, you should keep using your prescribed drops as usual. Stopping them could artificially raise your eye pressure and skew results.
What does a ‘borderline’ result mean?
A borderline result indicates that the visual field shows some changes, but they don’t yet meet the full criteria for glaucoma progression. Your doctor will likely repeat the test in a few months to see if the pattern persists.
Do cataracts affect visual field results?
Yes. A cloudy lens can block light, making the visual field appear worse. Your clinician may adjust the interpretation or repeat the test after cataract surgery.

Comments
Rajesh Singh
October 18, 2025 AT 12:54Taking your visual field test seriously is a moral duty to safeguard the precious canvas of your vision. The peripheral shadows it reveals are silent alarms, and ignoring them is tantamount to neglecting a dying ember. By following the prep steps-skipping caffeine, noting your meds-you honor the responsibility you owe your eyes. The data you feed the doctor isn’t just numbers; it’s a testament to your commitment to self‑care. Remember, glaucoma doesn’t ask for forgiveness, it only offers a chance for early action.
Albert Fernàndez Chacón
October 27, 2025 AT 23:54The Humphrey perimeter is a reliable workhorse; it maps the field with consistent precision. Keeping your head steady and pressing the button only when you truly see a flash yields clean data. If you’re nervous, think of the test as a brief conversation between you and the machine-no high stakes, just friendly measurement. Regular checks every six months keep the trend line smooth and the treatment plan on point.
Drew Waggoner
November 6, 2025 AT 11:54When the dim light flickers in the corner of your vision, the brain registers a whisper of existence that most of us never notice in daily life. That whisper is exactly what the visual field test captures, turning invisible loss into a tangible pattern. The process may feel tedious, but each click you make is a data point that builds a map of your retinal health. Even if you miss a flash, the software records a false negative that can be factored into the analysis. Over a series of tests, the mean deviation (MD) will trace the overall slope of your visual function. A steadily declining MD is a red flag that should prompt your doctor to intensify therapy. Conversely, a stable MD across multiple visits suggests that your current regimen is holding the disease at bay. Don’t be surprised if the technician mentions that you’ll need to sit still for five to ten minutes per eye. Your pupil may dilate slightly in response to the low‑intensity lights, which is normal and harmless. Caffeine or nicotine can constrict pupils and alter reaction times, which is why the pre‑test advice asks you to avoid them. If you wear glasses, you’ll usually be asked to remove them so the device can assess the naked eye. Some clinics employ frequency‑doubling technology as a quicker screen, but the Humphrey remains the gold standard for detailed assessment. When cataracts cloud the lens, the visual field may appear worse, so your doctor might order a cataract‑adjusted analysis. The graphical output, with its green, yellow, and red codes, is not just decorative; it highlights zones of loss at a glance. Ultimately, the test is a partnership-your cooperation and the machine’s precision together create a reliable portrait of your ocular future.
Mike Hamilton
November 15, 2025 AT 23:54i think u r right abot the test but also i feel like most docs dont explain the graphs well they just show a colorful map and say "good" or "bad" its confusing for us regular folks
Liberty Moneybomb
November 25, 2025 AT 11:54they never tell you that the big pharma labs push these tests to sell more meds, and the whole "early detection" hype is just a ploy to keep you hooked on expensive eye‑drops forever.
Brian Van Horne
December 4, 2025 AT 23:54Indeed, the Humphrey device remains the quintessential instrument for peripheral vision assessment.
Karla Johnson
December 14, 2025 AT 11:54Delving into the nuances of visual field metrics reveals just how intricate glaucoma management truly is; the mean deviation and pattern standard deviation are not mere numbers but reflections of localized neuronal loss that demand careful interpretation. When the glaucoma hemifield test flags asymmetry, it signals that the disease may be favoring one side of the retina, which can guide targeted therapeutic adjustments. Moreover, integrating OCT data with functional field results provides a composite view that bridges structural and functional decline, a synergy that many clinicians still overlook. Patients often underestimate the impact of systemic factors-blood pressure fluctuations, sleep apnea, even stress-on intraocular pressure, and consequently on visual field stability. Therefore, counseling should extend beyond drops to encompass lifestyle modifications that can subtly influence disease trajectory. Consistent follow‑up every six months is essential, yet the timing may need to be individualized based on trend analyses and patient compliance. In practice, fostering an open dialogue about these variables empowers patients to become active participants in preserving their visual horizon.
Janet Morales
December 23, 2025 AT 23:54while all that “integrated approach” sounds nice, most insurance plans won’t cover the extra OCT scans, leaving folks stuck with just the field test and a stack of pricey drops.
Alex Lineses
January 2, 2026 AT 11:54For anyone starting out, remember that the Reliability Indices-Fixation Loss, False Positives, and False Negatives-are your first checkpoint; values under 15% generally indicate a trustworthy test, so make sure the technician reviews those before you leave. If you notice elevated false positives, try to relax and avoid “anticipating” the light, as that can bias the results. Consistent medication adherence combined with stable visual field trends is the cornerstone of long‑term glaucoma control, so keep a log of your drops and schedule your next perimetry session well before the six‑month window closes.
Norman Adams
January 11, 2026 AT 23:54oh great, another lecture on “reliability indices”-because we all have time to become statisticians between our morning coffee and the inevitable retinal degeneration.