What You’re Seeing on Your Prescription Bottle
Open your prescription bottle. Look at the label. You’ll see two names - one big, one smaller. The big one? That’s the brand name, like Lipitor. The smaller one underneath? That’s the generic name: atorvastatin. They’re the same drug. Same active ingredient. Same effect. Same safety profile. But one costs $300 a month. The other? $4.
It’s not magic. It’s science. And it’s law. Since 1984, the U.S. Food and Drug Administration (FDA) has required that generic drugs prove they work exactly like their brand-name counterparts. That means identical active ingredients, same strength, same form - tablet, capsule, liquid - and same way your body absorbs it. The FDA doesn’t just trust the manufacturer. They demand proof. Bioequivalence tests show that the amount of drug in your bloodstream (AUC) and the peak level it reaches (Cmax) must fall within 80-125% of the brand-name version. That’s not a guess. It’s a strict, measurable standard.
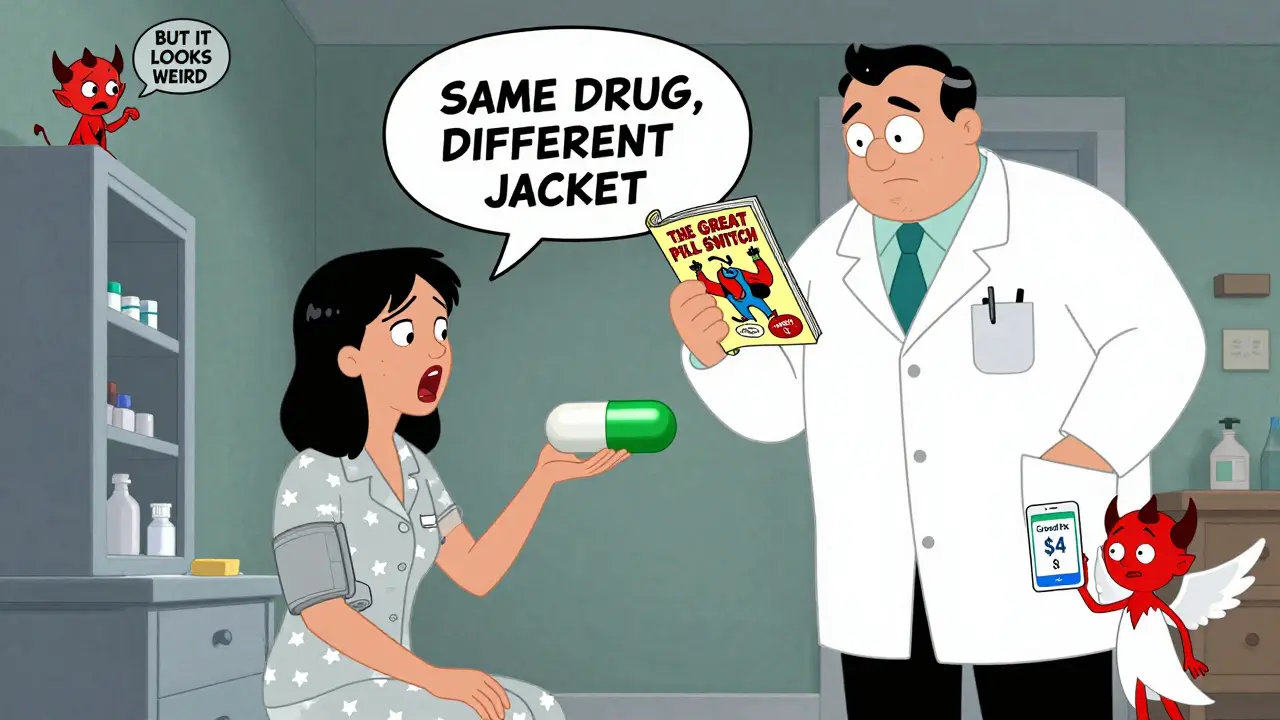
Why Do They Look Different?
Ever picked up a pill and thought, “This isn’t the same one”? You’re not wrong. It looks different. Maybe it’s blue instead of purple. Maybe it’s oval instead of round. Maybe it has a weird marking like “ATV 20” instead of “LIPITOR.” That’s not a mistake. That’s the law.
Trademark rules say generic manufacturers can’t copy the exact shape, color, or logo of the brand-name drug. So they change it. But here’s the catch: none of that affects how the drug works. The active ingredient - the part that lowers your cholesterol, treats your infection, or calms your anxiety - is chemically identical. The differences are in the fillers, dyes, and coatings. Those are called inactive ingredients. They help the pill hold together, dissolve properly, or look nice. But they don’t treat your condition.
That’s why 15% of medication errors involve patients mixing up pills because they look different. One woman in Perth told me her blood pressure med switched from a white oval to a green capsule. She stopped taking it for a week, convinced it wasn’t working. Her pharmacist had to sit down with her, show her the label, and explain: same drug. Same dose. Same result. She’s fine now. But she wasn’t alone.
Why Are Generics So Much Cheaper?
Brand-name drugs cost a fortune because the company had to pay for every step: discovering the molecule, running clinical trials, proving it’s safe, getting FDA approval. That process can cost over $2.6 billion per drug, according to Tufts Center for the Study of Drug Development. And that’s before marketing, advertising, or lobbying.
Generic manufacturers? They don’t do any of that. They don’t need to. The brand-name drug already proved it works. All they have to prove is that their version delivers the same amount of active ingredient the same way. That’s it. No new trials. No new patents. Just manufacturing. And because dozens of companies can make the same generic, competition drives prices down.
Result? You save 80-85%. Lipitor (brand) was $300 a month. Atorvastatin (generic)? $4. Sertraline (Zoloft) went from $450 to $5. That’s not a discount. That’s a revolution. From 2007 to 2016, generics saved the U.S. healthcare system $1.67 trillion. That’s not a number. That’s real money - money that kept people on their meds, out of hospitals, and off emergency rooms.

Who Makes the Generics?
Here’s something most people don’t know: about half of all generic drugs are made by the same companies that make the brand-name versions. Pfizer, Novartis, Merck - they all have generic divisions. They just slap a different label on it. So when you think you’re buying a “cheap” generic, you might actually be getting the exact same pill, just cheaper.
It’s not deception. It’s business. The brand company owns the patent. Once it expires, they can still profit by selling the same drug under a generic name. And since they already know how to make it, they can do it cheaper than a new player. That’s why some generics are more consistent than others - they come from the same factory.
When Generics Might Not Be the Best Choice
Most of the time, generics are perfect. But not always. There’s a small group of drugs called “narrow therapeutic index” (NTI) drugs. These are medicines where even tiny changes in blood levels can cause big problems. Think warfarin (Coumadin), lithium, or certain seizure meds. For these, some doctors still prefer the brand name - not because generics are unsafe, but because the margin for error is razor-thin.
The FDA says generics for NTI drugs still meet bioequivalence standards. But some prescribers, especially for patients with complex conditions, still choose brand names. That’s a medical decision. Not a quality issue. And it’s rare. Less than 1% of all medications fall into this category.
If you’re on one of these drugs and your pharmacy switches you to a generic, talk to your doctor. Don’t assume it’s dangerous. But do ask: “Is this one of those cases where consistency matters more?”
What the Label Really Says
Every prescription label must list both names. The brand name is usually bigger. The generic name is smaller, underneath. That’s the standard. The National Association of Boards of Pharmacy says 92% of labels follow this format. But here’s the thing: you don’t have to just accept it. You can ask for both names to be printed clearly on the bottle. Forty-one states require pharmacists to do this if you ask.
And if you’re confused? Ask your pharmacist. Seriously. They’re trained for this. University Hospitals found that just five minutes of counseling cuts patient confusion about generics by 67%. That’s huge. You’re not being annoying. You’re being smart.
Why People Still Don’t Trust Generics
Surveys show 32% of patients worry generics won’t work as well. Why? Because they look different. Because they cost less. Because someone on Reddit said their generic made them feel “weird.”
But here’s what the data says: 78% of patients who switch to generics report being satisfied - once they understand they’re getting the same drug. The “weird” feeling? Often comes from inactive ingredients. A dye, a filler, a coating. Some people are sensitive to those. It’s not the drug failing. It’s your body reacting to something else in the pill. Talk to your pharmacist. They can often switch you to a different generic brand - one with a different filler - and the problem disappears.
And yes, some people swear their brand-name drug “just worked better.” But in controlled studies, there’s no difference in outcomes. Perception isn’t proof. But it’s real. And it matters. That’s why education is key.
What’s Changing in 2026?
By 2026, 78% of all prescriptions in the U.S. will be generic - up from 90% of prescriptions already being filled with generics today. Why? Because more biologic drugs - complex medicines for cancer, arthritis, and diabetes - are losing patent protection. These aren’t pills. They’re injectables. But they’re still getting generic versions, called biosimilars. They’re not exact copies like traditional generics, but they’re close enough to save 15-30%.
Also, the Inflation Reduction Act of 2022 caps out-of-pocket drug costs for Medicare Part D at $2,000 a year starting in 2025. That’s going to push even more seniors toward generics. Why pay $200 for a brand if you can get the same thing for $5?
But there’s a risk. Over 80% of the active ingredients in pills - the actual medicine - come from China and India. Supply chain issues, like those during the pandemic, can cause shortages. The FDA is working on faster approvals under GDUFA III, aiming to cut approval times by 20% by 2027. But it’s a fragile system.
What You Should Do
- Always check your prescription label for both names - brand and generic.
- If you’re unsure, ask your pharmacist: “Is this the same as the brand?” They’ll show you the label and explain.
- Don’t stop taking a generic because it looks different. That’s normal.
- If you feel different after switching, talk to your pharmacist about inactive ingredients - not the active one.
- For NTI drugs like warfarin, ask your doctor if switching is safe for you.
- Use tools like GoodRx to compare prices. Often, the generic is cheaper even without insurance.
You’re not saving money because generics are inferior. You’re saving because the system works. The brand-name company paid the upfront cost. The generic company just copies it - legally, safely, and effectively. And you’re the one who benefits.


Comments
Chris & Kara Cutler
February 2, 2026 AT 00:21vivian papadatu
February 2, 2026 AT 08:35Also, the color change freaked me out at first - my old pill was blue, the new one was white. I thought I got the wrong med. Turns out, trademark rules force them to look different. Wild, right?
Rachel Liew
February 4, 2026 AT 03:34Jamie Allan Brown
February 4, 2026 AT 19:18Nicki Aries
February 5, 2026 AT 00:21Deep Rank
February 5, 2026 AT 21:34Naomi Walsh
February 5, 2026 AT 22:07Bryan Coleman
February 6, 2026 AT 01:54Naresh L
February 6, 2026 AT 10:01Sami Sahil
February 8, 2026 AT 06:36franklin hillary
February 9, 2026 AT 01:55Bob Cohen
February 9, 2026 AT 14:36Ishmael brown
February 10, 2026 AT 09:04Aditya Gupta
February 11, 2026 AT 18:48Nancy Nino
February 12, 2026 AT 10:27