Many people believe that generic drugs can contain anywhere from 80% to 125% of the active ingredient compared to the brand-name version. That’s not true. And this misunderstanding is why some patients refuse generics - even when they’re cheaper and just as safe. The 80-125% rule isn’t about how much drug is in the pill. It’s about how fast and how much of that drug gets into your bloodstream. Let’s clear up the confusion.
What the 80-125% Rule Actually Measures
The 80-125% range isn’t a tolerance for how much active ingredient a generic drug can have. It’s a statistical boundary for bioequivalence. That means: when you take a generic drug, your body absorbs it at a rate and to an extent that’s very close to the brand-name version. The FDA requires that the 90% confidence interval of the ratio between the generic and brand drug’s key measurements - AUC and Cmax - must fall entirely within 80% to 125%.
AUC stands for area under the curve. It tells you how much of the drug your body is exposed to over time - the total amount absorbed. Cmax is the highest concentration of the drug in your blood after taking it. That tells you how fast it gets absorbed. Both matter. A drug that gets absorbed too fast might cause side effects. One that’s too slow might not work at all.
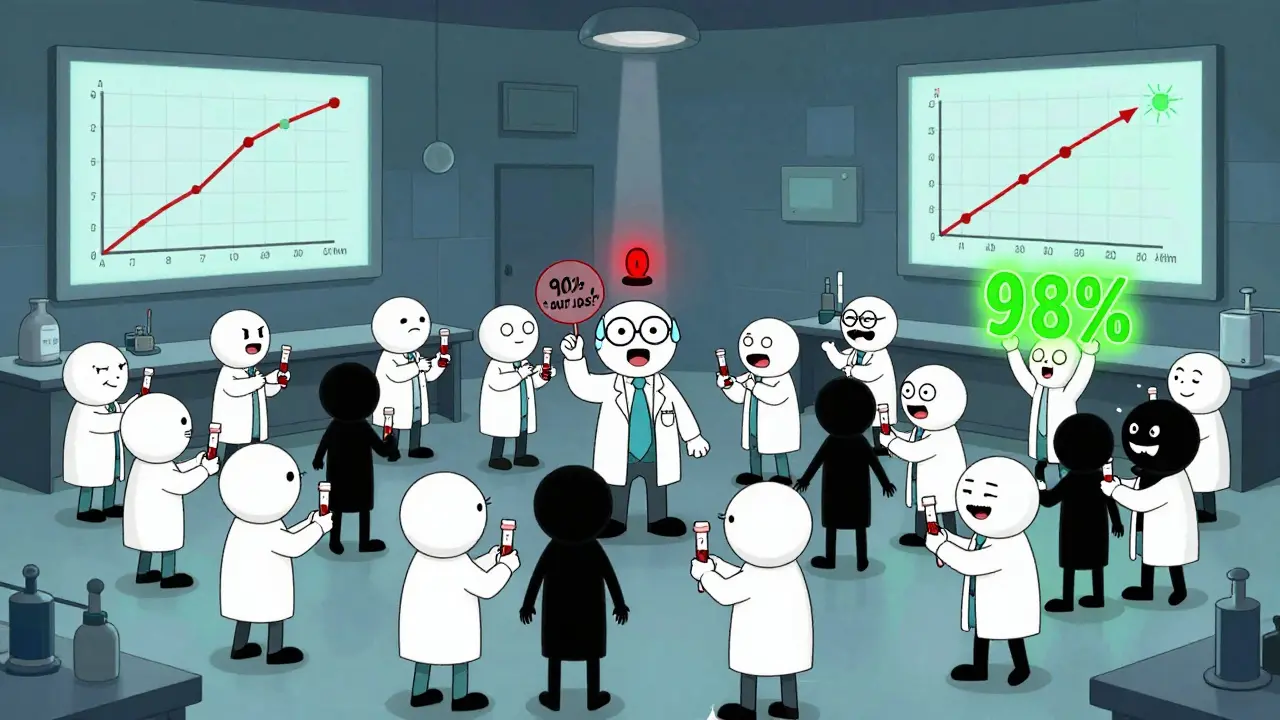
The FDA doesn’t just look at the average. They require the entire 90% confidence interval to stay within those bounds. That’s a big deal. It means even if the average is spot-on, if there’s too much variation between people, the drug fails. In practice, most approved generics land between 90% and 110% of the brand drug’s absorption. A 2008-2012 FDA analysis of over 2,000 studies showed 98% of generics had point estimates within 95-105%.
Why 80-125% and Not 90-110%?
You might wonder: why not just say ±10%? The answer is math - and biology.
Drug absorption data doesn’t follow a normal bell curve. It follows a log-normal distribution. That means differences in absorption are better measured on a logarithmic scale. On that scale, a 20% difference below 100% (80%) and a 20% difference above (125%) are symmetrical. Log(0.8) = -0.223, and exp(0.223) = 1.25. That’s why the range is 80-125%, not 80-120%. It’s not arbitrary. It’s based on how the human body actually processes drugs.
Think of it like this: if a brand drug gives you 100 units of exposure, a generic with 80 units might be fine - but only if every single person who takes it gets between 80 and 125. If even a few people get 75 or 130, the drug doesn’t pass. The 90% confidence interval acts like a safety net. It forces manufacturers to prove their product behaves consistently across many people.
How Bioequivalence Studies Work
Before a generic drug hits the shelf, it goes through a clinical study. Usually, 24 to 36 healthy volunteers take both the brand and generic versions in a crossover design - meaning half take the brand first, then the generic, and the other half reverse that order. Blood samples are taken every 15 to 30 minutes over 72 hours. Labs measure the concentration of the drug in plasma at each time point.
Those numbers get plugged into a statistical model. The geometric mean ratio of AUC and Cmax between the two drugs is calculated. Then, the 90% confidence interval is built. If that interval sits entirely between 80% and 125%, the drug is approved.
It’s not easy. Companies spend millions on these studies. And many fail. According to the FDA’s 2022 report, 32% of generic applications were incomplete - often because the bioequivalence data didn’t meet the standard. That’s why not every generic that’s submitted gets approved.
What About Drugs That Need to Be Exact?
Not all drugs are created equal. Some have a narrow therapeutic index - meaning even a small change in blood levels can cause harm or make the drug ineffective. Think warfarin, levothyroxine, or phenytoin.
For these, the FDA uses tighter standards. Since 2019, the acceptable range for certain narrow therapeutic index drugs is 90-111%. That’s a much smaller window. And it’s not just about the number. The FDA also requires more subjects in the study, more frequent blood draws, and sometimes replicate designs to account for higher variability.
Even then, real-world outcomes show generics work. A 2016 JAMA Internal Medicine study tracked over 2 million patients on generic cardiovascular drugs. No difference in heart attacks, strokes, or deaths between brand and generic users. Another study from the FDA’s Sentinel Initiative, covering 200 million patient records between 2015 and 2020, found no increase in adverse events with generics for 94% of drugs tested.
Why Do So Many People Still Doubt Generics?
Because the rule sounds scary. “80 to 125%? That’s a 45% range!” But that’s not what it means. It’s a statistical boundary, not a tolerance for variation in the pill. The average difference between brand and generic drugs is just 3.5%, according to FDA data.
Pharmacists hear this myth every day. A 2020 survey by the National Community Pharmacists Association found 78% of pharmacists explain the bioequivalence rule to patients at least once a week. And 63% said once they explained it, patient concerns disappeared.
Still, misinformation spreads. On Reddit and pharmacy student forums, you’ll find posts claiming generics can have “up to 25% less drug.” That’s false. The pill contains the same amount of active ingredient. The difference is in how your body absorbs it - and the system is designed to ensure that difference is tiny.

Generics Save Billions - and They Work
By 2022, generics made up 90% of all prescriptions filled in the U.S. - but only 23% of total drug spending. That’s a $373 billion savings in one year alone.
And it’s not just about cost. The FDA has approved over 800 generic drugs each year for the past few years. Most of them pass bioequivalence testing on the first try. And when they don’t, they’re not approved. No exceptions.
Healthcare providers know this. The Generic Pharmaceutical Association’s 2022 survey showed 97% of pharmacists prescribe generics as the first choice when available. Only 1.2% of prescriptions for brand drugs were due to concerns about generic effectiveness.
What’s Changing?
The FDA is working on new ways to test complex generics - like inhalers, topical creams, and long-acting injectables. For these, blood levels don’t always tell the whole story. That’s why they’re developing “model-informed drug development” tools using computer simulations to predict how a drug will behave in the body.
But for the vast majority of pills you take - antibiotics, blood pressure meds, antidepressants - the 80-125% rule remains the gold standard. It’s been used for over 30 years. It’s been tested in millions of patients. And it works.
The Supreme Court even upheld it in 2022. Justice Kavanaugh wrote that the FDA’s approach “has withstood three decades of real-world testing.” That’s not just regulatory jargon. It’s proof.
Bottom Line: Generics Are Safe, Effective, and Rigorously Tested
If your doctor prescribes a generic, you’re not getting a cheaper version of the drug. You’re getting the same drug, absorbed the same way, with the same results. The 80-125% rule isn’t a loophole. It’s a scientifically sound, statistically tight standard that ensures safety and effectiveness.
Don’t let the numbers scare you. The real story is simpler: generics work. They’ve saved lives. They’ve saved money. And they’ve passed the most rigorous testing in pharmaceutical history.
Does the 80-125% rule mean generic drugs can have 25% less or more active ingredient?
No. The active ingredient amount in a generic drug must be identical to the brand-name version. The 80-125% range refers to how much of that drug gets into your bloodstream - measured by AUC and Cmax - not how much is in the pill. The FDA requires the entire 90% confidence interval of these absorption measures to fall within that range, ensuring therapeutic equivalence.
Why is the range 80-125% and not 90-110%?
Because drug absorption data follows a log-normal distribution, not a normal one. On a logarithmic scale, a 20% decrease (80%) and a 20% increase (125%) are symmetrical around 100%. Using 90-110% would be statistically inappropriate and could miss real differences in absorption. The 80-125% range was chosen based on decades of pharmacokinetic research and expert consensus.
Are generics as safe as brand-name drugs?
Yes. The FDA requires generics to meet the same quality, strength, purity, and stability standards as brand-name drugs. Real-world data from over 2 million patients and 200 million records show no difference in effectiveness or safety between brand and generic versions for the vast majority of drugs. Adverse event rates are nearly identical.
Do all generic drugs follow the 80-125% rule?
Most do - but not all. For drugs with a narrow therapeutic index, like warfarin or levothyroxine, the FDA uses a tighter range: 90-111%. For complex products like inhalers or topical creams, bioequivalence may be assessed using different methods since blood levels don’t always reflect clinical effect. But for standard oral tablets and capsules, the 80-125% rule is universal.
Why do some doctors still prescribe brand-name drugs?
Sometimes it’s habit, or patient preference. Rarely, it’s because a patient had a bad reaction to a specific generic manufacturer’s version - though that’s usually due to inactive ingredients, not the active drug. In most cases, switching between generics from different manufacturers is safe. The FDA’s standards ensure all approved generics are therapeutically equivalent.
Can I trust a generic drug from another country?
Only if it’s approved by your country’s regulatory agency. The FDA only approves generics made in facilities that meet U.S. standards, whether they’re in the U.S., India, or elsewhere. Many international manufacturers supply FDA-approved generics. But buying unapproved generics online is risky - those products may not meet the 80-125% standard or any safety rules.


Comments
Rulich Pretorius
December 16, 2025 AT 17:13The 80-125% rule isn’t a loophole-it’s a mathematical safeguard. People panic because they hear ‘45% range’ and think it’s wild, but the log-normal distribution makes this the only sane way to measure absorption variability. The FDA didn’t pick this out of thin air; it’s decades of pharmacokinetic data distilled into a single, robust standard. Real-world outcomes confirm it: generics save billions without sacrificing safety.
What’s wilder is how little most people know about pharmacokinetics. We trust antibiotics, statins, even insulin generics without a second thought, yet this one metric triggers fear. It’s not about the pill-it’s about what your body does with it. And the system works.
Stop treating bioequivalence like a gamble. It’s the most scrutinized process in modern medicine.
Natalie Koeber
December 17, 2025 AT 00:20lol so the government says its safe but i saw a video on tiktok where some guy said the fillers in generics are actually microchips to track you. also why do brand name drugs cost 10x if theyre the same? something fishy here. i dont trust big pharma or the fda. they’re all in bed together. my cousin took a generic and felt ‘off’ for 3 days. coincidence? i think not.
also why do they use the word ‘bioequivalence’? sounds like corporate jargon to make us feel better. i’m not buying it. #GenericConspiracy
Thomas Anderson
December 18, 2025 AT 17:38It’s not about the pill. It’s about your body. If the drug gets into your blood the same way, you’re getting the same effect. The active ingredient? Same amount. The absorption? Same range. The results? Same outcomes. Millions of people use generics every day. If they were dangerous, we’d know. The data’s there. The science’s solid. Stop overthinking it.
Just take the generic. Save money. Feel better. Done.
Sarthak Jain
December 20, 2025 AT 07:41Man, I used to think the same thing-80-125% sounded like a wild range. But after studying pharmaco kinetics in med school, I realized it’s all about the log scale. You can’t treat absorption like a linear thing. The body doesn’t work that way. A 20% drop isn’t the same as a 20% rise in linear terms-it’s exponential. That’s why 80 and 125 are symmetrical on a log scale.
And yeah, most generics land between 95-105%. The FDA’s got this locked down. I’ve seen the raw data. It’s not magic. It’s math. And math doesn’t lie.
Also, if your doctor prescribes a generic, they’re not cutting corners. They’re being smart.
Sinéad Griffin
December 21, 2025 AT 10:04AMERICA STILL THE BEST IN PHARMA. WE’RE THE ONLY COUNTRY THAT TESTS THIS HARD. OTHER COUNTRIES JUST GIVE YOU ANYTHING. I’M SO PROUD TO BE AMERICAN. 🇺🇸💪🇺🇸
Also, if you don’t trust generics, you’re basically saying you trust India more than the FDA. And that’s just sad.
jeremy carroll
December 22, 2025 AT 20:00Just wanted to say thanks for explaining this so clearly. I’ve been on a generic blood pressure med for 5 years and never questioned it. But now I actually understand why it works. My mom was freaking out about it last week-now I’ve got the data to show her. Seriously, this post deserves more attention. Keep doing the good work.
Also, generics saved me $800 last year. That’s a whole month of groceries. Win-win.
Edward Stevens
December 23, 2025 AT 10:51So let me get this straight: the FDA requires 90% of the population to absorb the drug within a range that sounds like a casino payout… and we’re supposed to be comforted by that?
Meanwhile, my cousin’s generic thyroid med made her feel like a zombie for six months. She switched back to brand and suddenly had energy again. Coincidence? Or is the ‘98% success rate’ just a nice way of saying ‘we let 2% of people suffer silently’?
Also, why do they even call it ‘bioequivalence’? Sounds like something a corporate lawyer came up with after a three-martini lunch.
Alexis Wright
December 23, 2025 AT 12:35Let’s be brutally honest: the 80-125% rule is a political compromise disguised as science. The FDA didn’t choose this because it’s perfect-it’s because it’s the lowest bar that lets generics flood the market. The fact that 32% of submissions fail? That’s not a sign of rigor-it’s a sign that most manufacturers are cutting corners until they barely scrape by.
And don’t get me started on the ‘98% within 95-105%’ stat. That’s cherry-picked. What about the outliers? The people whose Cmax is 130%? They’re not in the average. They’re the ones having strokes or seizures because their blood levels spiked. But hey, statistically speaking, they’re just noise.
This isn’t science. It’s capitalism with a lab coat.
Dwayne hiers
December 24, 2025 AT 13:25For those still confused: AUC is the total exposure over time. Cmax is the peak concentration. The 90% CI must lie entirely within 80–125%. That means even the 5th and 95th percentiles of the population are covered. It’s not about the mean-it’s about the distribution. And yes, it’s log-normal because plasma concentration curves are inherently multiplicative, not additive.
Also, the FDA’s 2022 report shows that for drugs with narrow therapeutic windows, the range is tightened to 90–111%. That’s not an afterthought-it’s a critical safeguard. The system adapts based on risk. That’s not incompetence. That’s precision.
Tim Bartik
December 26, 2025 AT 06:05Okay but what if the generic is made in a factory in Mumbai with a guy named Rajesh who’s got a 3rd grade education and his only tool is a hammer and a prayer? I’ve seen the documentaries. They use flour as filler. I’m not taking some cheap knockoff that smells like burnt toast. You think the FDA inspects every batch? LOL. I’d rather pay extra and sleep at night.
Also, why do brand names still exist if generics are the same? BECAUSE THEY’RE BETTER. Duh.
Wade Mercer
December 27, 2025 AT 07:27People who fear generics are the same people who think vaccines contain microchips and that the moon landing was faked. The science is settled. The data is public. The FDA doesn’t approve drugs based on opinion. They approve them based on statistical rigor. If you don’t trust the system, don’t take any medication. But don’t pretend your fear is rational. It’s not. It’s ignorance dressed up as caution.
Jonny Moran
December 29, 2025 AT 03:10I’m from South Africa and we rely heavily on generics here. Our public health system wouldn’t survive without them. I’ve seen patients on generics for HIV, TB, hypertension-lives saved, families kept together. The science isn’t perfect, but it’s the best we’ve got. And it works.
Don’t let fear of numbers blind you to the real impact: access. A generic that costs $5 instead of $50 means someone takes their meds. That’s not a compromise. That’s justice.
Daniel Thompson
December 30, 2025 AT 14:59Just a quick note: I work in a hospital pharmacy. Every day, I see patients refuse generics because they ‘don’t trust them.’ I explain the 80-125% rule. I show them the FDA reports. I tell them about the 2 million patient study. And 90% of them say, ‘Oh. I didn’t know that.’
It’s not about the science. It’s about communication. We need better public education-not more regulation. People aren’t irrational. They’re just uninformed.