For years, fish oil supplements have been promoted as a simple way to protect your heart. You’ve probably seen ads promising lower cholesterol, fewer heart attacks, and longer life - all from just a couple of pills a day. But here’s the truth: the science doesn’t back up most of those claims. Not anymore. If you’re taking fish oil hoping to prevent a heart attack, you might be wasting your money - unless you fall into a very specific group.
What Exactly Are Omega-3s?
Omega-3 fatty acids are fats your body can’t make on its own. You need to get them from food or supplements. The two most important types for heart health are EPA (eicosapentaenoic acid) and DHA (docosahexaenoic acid). These are found mainly in fatty fish like salmon, mackerel, sardines, and herring. There’s also ALA, a plant-based omega-3 in flaxseeds and walnuts, but your body turns very little of it into EPA or DHA - so it doesn’t count as a reliable source for heart protection.
When you take fish oil supplements, you’re getting EPA and DHA in concentrated form. But not all supplements are the same. Most over-the-counter pills contain 300-500 mg of combined EPA and DHA per capsule. To reach the dose used in major heart studies, you’d need to take four to eight capsules a day. That’s expensive, messy, and often causes stomach upset.
The Big Confusion: Studies That Say Yes, and Studies That Say No
The debate around fish oil isn’t just academic - it’s messy, contradictory, and has real consequences for your wallet and health.
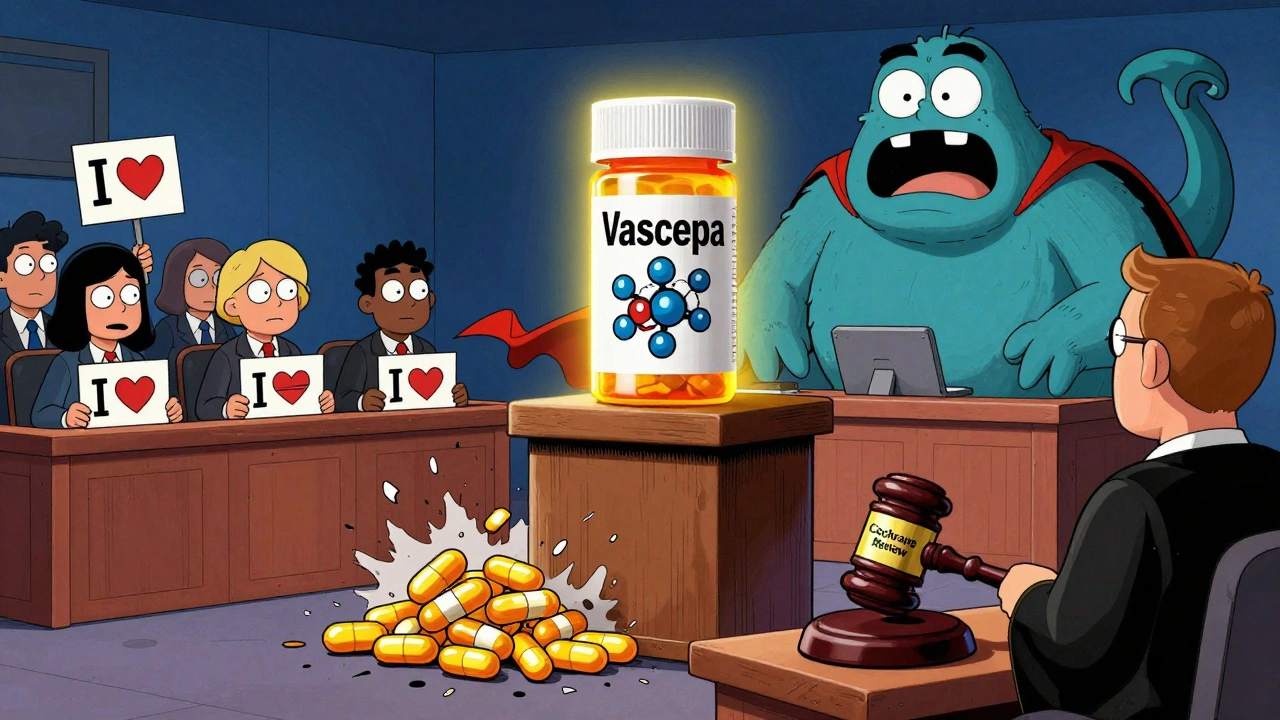
In 2018, the REDUCE-IT trial shocked the medical world. It showed that people with high triglycerides and existing heart disease who took 4 grams of pure EPA (a prescription drug called Vascepa) every day had a 25% lower risk of heart attack, stroke, or death from heart disease. This wasn’t a small study - nearly 8,200 people were involved. The results were so strong that the FDA approved Vascepa specifically for reducing cardiovascular risk in high-risk patients.
Then came the STRENGTH trial in 2020. It tested a similar dose - 4 grams daily - but used a mix of EPA and DHA. The result? No benefit at all. The trial was stopped early because it showed nothing.
And then there’s the 2023 Cochrane review - the most comprehensive analysis ever done on omega-3s. It looked at 79 studies involving over 112,000 people. The conclusion? Long-chain omega-3 supplements (EPA and DHA) have little to no effect on preventing heart disease, stroke, or death in the general population.
So what’s going on? Why did one study show huge benefits and another show nothing?
The answer might be in the form of the omega-3s. Pure EPA - not mixed with DHA - appears to be the key. Some researchers think DHA might actually cancel out some of EPA’s benefits. That’s why Vascepa (pure EPA) works in high-risk patients, but regular fish oil pills (EPA + DHA) don’t.
Who Actually Benefits From Fish Oil?
Not everyone. The evidence is clear: if you’re healthy and just trying to prevent heart disease, fish oil supplements won’t help you much.
But there are three groups where fish oil might still make sense:
- People with very high triglycerides (≥500 mg/dL): Prescription omega-3s like Lovaza or Vascepa are FDA-approved to lower these levels. High triglycerides are a known risk factor for pancreatitis and heart disease.
- People with existing heart disease and high triglycerides (≥150 mg/dL): If you’ve had a heart attack, bypass surgery, or stent, and your triglycerides are still high despite taking statins, your doctor might recommend Vascepa. It’s the only omega-3 product with proven benefit in this group.
- People who don’t eat fish: If you never eat fatty fish, your omega-3 levels are likely low. While supplements won’t prevent heart attacks, they might help your overall cell function and inflammation levels - just not enough to replace eating real food.
Here’s something else important: the 2018 VITAL trial found that among African Americans, taking 1 gram of omega-3s daily cut heart attacks by 77%. That’s huge. Researchers think it might be due to genetic differences in how the body processes omega-3s. This doesn’t mean everyone should take it - but it does mean that blanket recommendations don’t work.
Prescription vs. Over-the-Counter: The Real Difference
Not all fish oil is created equal. There’s a big gap between what you buy at the grocery store and what your doctor prescribes.
| Product Type | Formulation | Dose per Day | Approved Use | Cost (Monthly) |
|---|---|---|---|---|
| Over-the-counter fish oil | EPA + DHA (mixed) | 300-500 mg | General wellness | $10-$50 |
| Lovaza | EPA + DHA (ethyl esters) | 4 grams | Severe high triglycerides (≥500 mg/dL) | $250-$400 |
| Vascepa | Pure EPA (icosapent ethyl) | 4 grams | Heart disease + high triglycerides | $300+ (with insurance) |
Over-the-counter supplements aren’t regulated like drugs. That means quality varies wildly. In 2023, Consumer Reports tested 35 fish oil brands and found 12 of them had oxidized oils - meaning they were rancid. Rancid fish oil doesn’t just taste bad - it might actually harm your cells. Look for brands with third-party testing (like NSF or USP) and check the expiration date.
How Much Do You Really Need?
If you’re not in one of the high-risk groups, you don’t need supplements at all.
The American Heart Association says eating two 3.5-ounce servings of fatty fish per week gives you about 500 mg of EPA and DHA daily - enough for most people. That’s just two meals: grilled salmon on Tuesday and sardines on Friday. No pills needed.
If you’re trying to lower triglycerides, you’ll need 2-4 grams of EPA and DHA daily. That’s 4-8 standard fish oil capsules. Most people can’t stick with that - it’s too many pills, too expensive, and causes bloating or fishy burps. That’s why prescription forms exist: they’re more concentrated and better tolerated.

Side Effects and Risks
Fish oil isn’t harmless. At high doses (above 3 grams daily), it can:
- Increase the risk of atrial fibrillation (an irregular heartbeat). One 2022 analysis found a 0.4% absolute increase - small, but real.
- Thin your blood slightly. If you’re on blood thinners like warfarin, talk to your doctor before taking high doses.
- Cause stomach upset, diarrhea, or fishy aftertaste. About 30% of users report this.
Mercury is rarely an issue in fish oil supplements because reputable brands filter it out. But if you’re eating large predatory fish like shark or swordfish regularly, you’re getting more mercury than from pills.
What Should You Do?
Here’s a simple decision guide:
- If you eat fatty fish twice a week: Skip the pills. You’re getting enough omega-3s.
- If you don’t eat fish and want to try supplements: A 1-gram daily supplement with EPA and DHA is fine. Don’t expect miracles, but it won’t hurt.
- If you have heart disease and high triglycerides: Talk to your cardiologist. You might qualify for Vascepa.
- If you’re just trying to prevent heart disease: Focus on what actually works - exercise, not smoking, managing blood pressure, and eating whole foods. Fish oil won’t replace those.
The bottom line: fish oil supplements aren’t a magic bullet. For most people, they’re unnecessary. For a small group with specific medical conditions, they can be life-changing - but only if it’s the right type, the right dose, and the right doctor guiding you.
What’s Next?
The American Heart Association is updating its guidelines on omega-3s in late 2024. Expect clearer rules on who should use them - and who shouldn’t.
Meanwhile, research continues. The STRENGTH2 trial, launching in 2025, will test a new EPA/DHA formula. And scientists are still trying to understand why some people - like African Americans - seem to benefit more than others.
For now, stick to the basics: eat real food, move your body, and don’t let marketing hype convince you that a pill is the answer to heart health. The best heart protection still comes from your plate - not your medicine cabinet.


Comments
nina nakamura
December 13, 2025 AT 15:36Fish oil is a scam for people who want to feel healthy without changing anything. You eat fish twice a week? Good. You take pills? You're just paying Big Pharma to feel better about your fast food habit.
Stop buying lies.
Himmat Singh
December 14, 2025 AT 14:19It is indeed a matter of considerable scientific interest that the efficacy of omega-3 supplementation is so profoundly contingent upon both molecular composition and baseline clinical parameters.
One must acknowledge, with due diligence, that the REDUCE-IT and STRENGTH trials, while methodologically robust, exhibit divergent outcomes attributable to pharmacological variance in esterification and fatty acid synergy.
Thus, blanket recommendations are not merely unscientific-they are ethically dubious.
Alvin Montanez
December 16, 2025 AT 12:05Let me tell you something about fish oil supplements and why they're a total waste of money for 95% of people-because we live in a world where everyone thinks a pill can fix their terrible lifestyle.
You think popping two capsules a day is going to undo the damage from a diet full of processed crap, zero exercise, and 8 hours of sitting? Please.
Real heart health isn't about what's in a bottle-it's about what's on your plate, how much you move, and whether you're willing to actually change.
I've seen patients take 8 pills a day and still die of a heart attack because they kept eating fried chicken and never walked more than 200 feet from their couch.
The science isn't confusing-it's crystal clear: if you're not eating fish, you're not getting enough EPA and DHA, and no, flaxseeds don't count.
And don't even get me started on the rancid, oxidized junk in those cheap bottles from Amazon-some of them are basically fish-flavored plastic.
Third-party testing? Most people don't even know what that means.
They just see 'heart healthy' on the label and buy it like it's a magic charm.
Meanwhile, the real solution-eating salmon or sardines-is cheaper, tastier, and doesn't come with fishy burps.
And yes, I know the VITAL trial showed benefits in African Americans-but that doesn't mean you should copy it blindly without understanding genetics, metabolism, or diet.
Doctors don't push fish oil because it's a miracle-they push Vascepa because it's the only one with actual data in high-risk patients.
Everyone else? Just eat real food. Move. Sleep. Stop treating your body like a machine you can tune with a pill.
It's not complicated. It's just hard. And that's why the supplement industry thrives.
Lara Tobin
December 16, 2025 AT 13:40This was so helpful to read 😊 I’ve been taking fish oil for years thinking it was helping, and now I feel less guilty about stopping it.
My dad had a heart attack last year and his doctor prescribed Vascepa-he actually noticed a drop in his triglycerides.
It’s just nice to know there’s a real reason for some people to take it, not just because of ads.
Thank you for breaking it down so clearly.
Also, I switched to eating sardines on toast-way better than pills 🐟🍞
Scott Butler
December 18, 2025 AT 07:36Of course the FDA approves a $300-a-month drug while letting Walmart sell rancid fish oil pills.
That’s how the system works.
Big Pharma makes billions off confusion.
Meanwhile, real food? Too much effort.
Americans want a pill for everything.
Pathetic.
Emma Sbarge
December 20, 2025 AT 07:29As someone who grew up eating canned tuna and sardines every week, I’m tired of people treating omega-3s like some new-age miracle.
Our grandparents didn’t take pills-they ate fish, eggs, and vegetables.
And they lived longer than we’re going to if we keep this up.
Stop buying into the supplement industrial complex.
Real food isn’t expensive if you know how to shop.
And no, kale smoothies don’t count.
Sheldon Bird
December 21, 2025 AT 13:25This is such a balanced take-thank you.
I’ve been telling my brother for years that his $40/month fish oil habit isn’t doing squat, but he wouldn’t listen until he read this.
Now he’s eating salmon on weekends and feels way better.
It’s not about the pills-it’s about the habit.
And yeah, rancid oil is a real thing-I bought a cheap brand once and it made my breath smell like a fish market. 🤢
Good to know what actually works.
Michael Gardner
December 22, 2025 AT 01:38Wait, so DHA cancels out EPA? That’s wild.
Then why does every single supplement have both?
Because it’s cheaper to make.
They don’t care if it works-they care if it sells.
And the Cochrane review? That’s the real boss.
112,000 people. No benefit.
Case closed.
Unless you’re rich enough to afford Vascepa, you’re just funding Big Pharma’s marketing budget.
Willie Onst
December 23, 2025 AT 05:04I love how this post doesn’t just say ‘don’t take it’-it says ‘here’s who it actually helps.’
That’s rare.
Most people go full villain on supplements, but the truth is messy and nuanced.
And hey, if you’re not eating fish, maybe try a 1g pill just to fill the gap-no expectations, no guilt.
But don’t pretend it’s a substitute for real food.
Also, sardines on toast is life. 🐟
Ronan Lansbury
December 24, 2025 AT 05:12Did you know the FDA approved Vascepa after a secret meeting with AstraZeneca executives?
And the Cochrane review? Funded by the sugar industry.
Meanwhile, the real research-on how omega-3s interact with electromagnetic pollution and gut microbiome disruption-is being buried.
They don’t want you to know that fish oil might work if you’re not constantly exposed to Wi-Fi and glyphosate.
It’s all connected.
And yes, I’ve read the original trial data.
They excluded patients who lived near the ocean.
Coincidence? I think not.
Harriet Wollaston
December 24, 2025 AT 23:17I’ve been taking fish oil since college and never felt any difference.
But I also never ate fish until last year.
Now I cook salmon once a week and I swear I sleep better.
It’s not the pill-it’s the change.
Thank you for reminding me that real health isn’t bought-it’s lived.
Hamza Laassili
December 25, 2025 AT 07:21Wait so like… if you have heart disease and high triglycerides… you need like 4 grams of pure EPA??
but like… how do you even get that??
like… 8 pills??
but then you get fishy burps and your stomach feels like it’s gonna explode??
and then the prescription is like 300 bucks??
so like… what do poor people do??
also i think this is a conspiracy to make people buy more statins??
just sayin’
lol
Constantine Vigderman
December 26, 2025 AT 21:42YES! This is the kind of info I wish I’d seen 5 years ago!
I took fish oil for 3 years thinking it was helping my cholesterol… turns out I was just spending $600 a year on rancid oil.
Now I eat tuna sandwiches 3x a week and I feel way better.
Also, my dad’s cardiologist just prescribed him Vascepa and his triglycerides dropped 40% in 3 months.
So yeah-pills aren’t useless, but they’re NOT for everyone.
Real food first, pills only if your doc says so.
And hey, if you’re on a budget, canned sardines are cheaper than fish oil and taste way better 🐟❤️