Why corticosteroids spike your blood sugar
When you take corticosteroids like prednisone or dexamethasone, your body doesn’t just fight inflammation-it also starts flooding your bloodstream with sugar. This isn’t a side effect you can ignore. About 20-50% of people on high-dose steroids develop high blood sugar, even if they’ve never had diabetes before. It’s not rare. It’s predictable. And it’s dangerous if left unchecked.
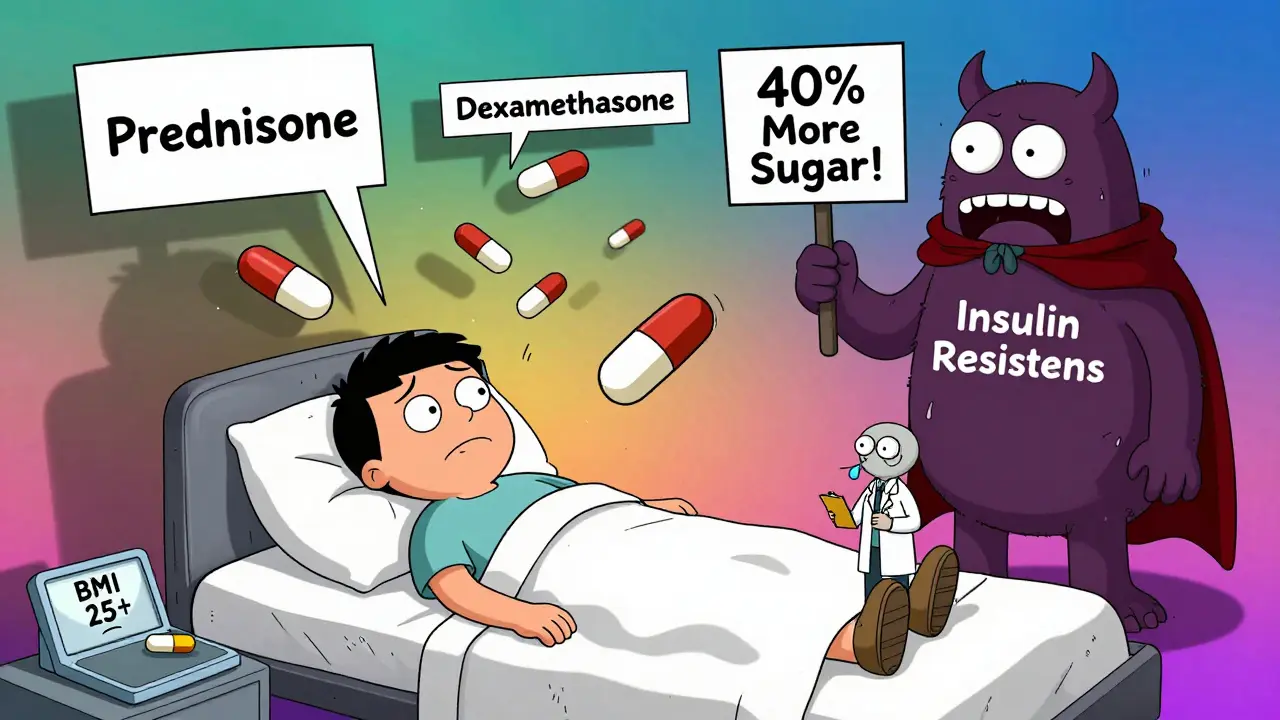
The problem isn’t just about eating too much sugar. Corticosteroids mess with your body’s natural glucose control in four key ways. First, your liver starts making more glucose-up to 40% more-by turning fat and protein into sugar. Second, your muscles stop responding to insulin, so glucose can’t get inside them to be used for energy. That’s called insulin resistance, and it’s worse in people who are overweight or over 50. Third, your fat cells break down faster, spilling free fatty acids into your blood, which makes insulin resistance even worse. Fourth, your pancreas slows down insulin production by 20-35%, because steroids block the signals that tell beta cells to release insulin.
This isn’t type 2 diabetes. It’s steroid-induced diabetes. And it behaves differently. Blood sugar doesn’t creep up slowly. It can spike within 24 to 48 hours after starting steroids, especially if you’re on a high dose. That’s why many patients don’t notice anything until they’re already in the hospital with dangerously high glucose levels.
Who’s most at risk?
Not everyone on steroids gets high blood sugar. But some people are far more likely to. If you’re taking prednisone at 7.5 mg or higher daily, your risk jumps by 3.2 times. Dexamethasone? Even worse-it’s six to eight times more likely to cause hyperglycemia than prednisone at the same anti-inflammatory dose. Age matters too. If you’re over 50, your risk nearly triples. Being overweight (BMI ≥25) adds another 2.5 times the risk. Family history of diabetes? That’s a 2.7-fold increase. And if you had gestational diabetes before? Your risk is over four times higher.
People with kidney problems are also at serious risk. If your eGFR is below 60, you’re almost four times more likely to develop steroid-induced hyperglycemia. That’s because your kidneys can’t clear excess glucose as well. And here’s something most patients don’t know: the longer you’re on steroids, the worse it gets. Every week beyond the first two increases your risk by 12%. Each extra 5 mg of prednisone? Another 18% higher chance of high blood sugar.
And it’s not just the dose. The timing matters too. Most steroids are taken in the morning. But the peak blood sugar spike doesn’t happen right away. It hits 4 to 8 hours later. That’s why checking your glucose only before breakfast might miss the worst part of the day.
What does it feel like?
Symptoms can be subtle-or they can hit you hard. About 60% of people notice something’s off. You might feel unusually thirsty, drinking more water than usual. You’ll be peeing more often, sometimes waking up at night. Fatigue hits hard-not just tired, but drained. Headaches, blurred vision, and a strange metallic taste in your mouth are common. But here’s the catch: 40% of cases show no symptoms at all. That’s why routine blood sugar checks are critical, especially if you’re on high-dose steroids.
And it’s easy to confuse steroid side effects with high blood sugar. Increased hunger? That’s common with steroids. Weight gain? That’s expected. Mood swings? Everyone blames the meds. But these are also signs of high glucose. One patient in a Reddit thread summed it up: “I thought I was just gaining weight from the steroids. Turns out I was diabetic.”
Many patients report being blindsided. A 2023 survey of diabetes forums found that 68% of people weren’t warned by their doctor about this risk. If you’re starting steroids, ask: “Will this affect my blood sugar?” Don’t wait for symptoms. Ask for a baseline glucose test before you begin.
How doctors monitor and treat it
Monitoring is the first line of defense. If you’re on prednisone at 20 mg or higher daily, your doctor should check your blood sugar at least twice a day-before breakfast and two hours after your largest meal. Some hospitals use continuous glucose monitors (CGMs) for patients in intensive care. The goal? Keep fasting glucose under 140 mg/dL (7.8 mmol/L) and random readings under 180 mg/dL (10.0 mmol/L).
For people with existing type 2 diabetes, insulin needs often jump by 50-100% during steroid treatment. That’s not a mistake-it’s expected. Your body is fighting two battles at once: inflammation and high glucose.
The go-to treatment? Basal insulin. It’s long-acting and works steadily through the day to handle the liver’s sugar overload. For every 10 mg increase in prednisone above 20 mg, doctors often raise basal insulin by 20%. Rapid-acting insulin is added for meals, usually 1 unit per 5 to 10 grams of carbs. Some patients do well with premixed insulin, but that’s less flexible if steroid doses change.
Oral meds like metformin help a little with insulin resistance, but they don’t fix the insulin shortage. Sulfonylureas (like glipizide) can force the pancreas to release more insulin-but they’re risky. When steroids are tapered, your blood sugar drops fast, and sulfonylureas can cause dangerous lows. In fact, 37% of hypoglycemia events in steroid patients happen because these drugs weren’t stopped or reduced in time.
What happens when you stop the steroids?
This is where most patients get confused. Steroid-induced diabetes usually goes away-fast. Once you stop taking the steroid, your blood sugar typically returns to normal in 3 to 5 days. But here’s the trap: many people keep taking diabetes meds because they assume they still have diabetes. That’s dangerous.
One study found that 63% of patients kept using insulin or pills long after their steroids were gone. That led to repeated low blood sugar episodes, falls, confusion, and even hospital visits. Your doctor should schedule a follow-up glucose test within a week of stopping steroids. If your levels are normal, most medications can be stopped. No need for lifelong treatment-unless you had prediabetes or another risk factor to begin with.
That’s why education matters. If you’re told, “You have diabetes,” ask: “Is this because of the steroids? Will it go away?” Don’t accept a diagnosis without context.

New tools and future directions
There’s progress on the horizon. A new mobile app called STEROID-Glucose, launched in 2023 by the European Association for the Study of Diabetes, helps patients and doctors adjust insulin doses in real time based on steroid type and dose. In early testing, it cut hyperglycemic events by 32%.
Researchers are also testing GLP-1 receptor agonists (like semaglutide) for steroid-induced hyperglycemia. Early data from the NIH’s GLUCO-STER trial shows these drugs cause 28% fewer low blood sugar episodes than insulin, because they only work when glucose is high. That’s a big advantage when steroid doses are changing daily.
The future might even avoid the problem altogether. Scientists are developing new steroids that fight inflammation without triggering sugar spikes. One experimental compound, XG-201, reduced hyperglycemia by 65% compared to prednisone in phase II trials-while keeping the same anti-inflammatory power.
But right now, the biggest challenge isn’t the science. It’s awareness. Steroid use is growing fast-especially in cancer care, like CAR-T therapy, where 75-85% of patients develop high blood sugar. By 2030, steroid-induced diabetes could become the third most common cause of secondary diabetes. That’s why every doctor prescribing steroids needs to think about glucose. And every patient needs to ask: “Will this affect my blood sugar?”
What you can do today
- Ask your doctor for a fasting blood glucose test before starting steroids.
- If you’re on 7.5 mg prednisone or more, request a glucose monitoring plan-don’t wait for symptoms.
- Check your blood sugar twice daily: before breakfast and 2 hours after your largest meal.
- Don’t assume high blood sugar means you have permanent diabetes. Ask if it’s steroid-related.
- When steroids are tapered, talk to your doctor about adjusting or stopping diabetes meds.
- Use a logbook or app to track your glucose, steroid dose, and meals. Patterns matter.
Steroids save lives. But they can also cause serious harm if blood sugar isn’t managed. You don’t need to avoid them. You just need to be prepared.


Comments
Nicholas Urmaza
January 16, 2026 AT 09:49Look I don't care how fancy the science is if your doctor doesn't warn you about this before handing you a prescription for prednisone they're failing you. I was on 40mg for a month and didn't know my glucose was at 320 until I passed out in the grocery store. They told me I had diabetes. Turns out it was just the steroids. I got off them and my numbers dropped like a rock in two days. Stop normalizing this. Ask the question before you start the med. It's not optional.
RUTH DE OLIVEIRA ALVES
January 17, 2026 AT 20:04It is imperative to underscore the clinical significance of steroid-induced hyperglycemia as a iatrogenic condition that demands proactive monitoring. The physiological mechanisms elucidated herein-namely hepatic gluconeogenesis augmentation, peripheral insulin resistance, and beta-cell suppression-are well-documented in endocrinological literature. It is, therefore, a professional obligation for prescribing clinicians to initiate baseline glycemic screening and to establish a structured glucose monitoring protocol prior to initiating corticosteroid therapy. Patient education must be systematic, not anecdotal.
Nilesh Khedekar
January 18, 2026 AT 15:24Ohhh so now we're blaming doctors for not telling you that steroids turn you into a walking sugar factory?? Wow. I'm shocked. Next you'll tell me that breathing oxygen causes your lungs to get wet. And let me guess-you didn't read the 12-page pamphlet they gave you with the prescription?? Oh wait-you didn't even ask. Typical. You want to be told everything like a toddler. Go get a PhD in reading medication inserts before you cry foul.
Jami Reynolds
January 18, 2026 AT 21:34Did you know that the pharmaceutical industry funds 92% of endocrinology research? And that the FDA approved dexamethasone for COVID without long-term glucose studies? This isn't just side effects-it's a silent campaign to push people into lifelong insulin dependency. Look at the timing: right after the rise of CGM companies. Coincidence? I think not. They want you dependent. They want you scared. And they want your data. Check your insulin vials for microchips. I'm not joking.
Crystel Ann
January 20, 2026 AT 12:36I had a friend on high-dose steroids after a transplant and no one mentioned blood sugar until she was in the ER. It was terrifying. But she found a nurse who taught her how to log her meals and glucose levels, and that made all the difference. You don’t have to figure it out alone. There are people who can help-if you speak up. Just ask. It’s okay to be scared. Just don’t stay silent.
Nat Young
January 22, 2026 AT 09:15Let me break this down for you. The article says 20-50% get high blood sugar. But 68% weren't warned? That math doesn't add up unless the 20-50% is a subset of the 68%. Also, who measured the 40% increase in liver glucose production? Was it a controlled trial or a mouse model? And why is dexamethasone 'worse' than prednisone? Is that based on mg-to-mg equivalence or anti-inflammatory potency? And what about the 37% hypoglycemia rate from sulfonylureas-was that in patients who tapered steroids properly or did they just keep dosing? This feels like cherry-picked stats wrapped in a lab coat.
Niki Van den Bossche
January 23, 2026 AT 10:51Ah, the beautiful, brutal ballet of endocrine sabotage-corticosteroids, those golden harbingers of inflammation’s annihilation, also orchestrate a symphony of metabolic dissonance. The liver, once a prudent steward of glucose, becomes a frenzied alchemist, transmuting protein and lipid into molten sugar. The muscles, once receptive to insulin’s gentle whisper, now slam the door shut in existential rebellion. And the pancreas? It weeps in silence, its beta cells silenced by molecular muzzles. This isn't diabetes-it's a metaphysical betrayal of homeostasis. We are not merely patients; we are collateral in the war against cytokines. And yet, the solution? Insulin. The same molecule that once kept us whole, now the chains that bind us. The irony is not lost on those who’ve tasted the metallic aftertaste of hyperglycemia-it tastes like betrayal dressed in white coats.
Jan Hess
January 25, 2026 AT 05:04Good breakdown. I’m a nurse and I’ve seen this a hundred times. Patients get scared when their numbers spike and think they’re diabetic for life. But when you explain it’s temporary and help them track it, most of them breathe a huge sigh of relief. The key is early checks and not waiting for symptoms. I always tell my patients: ‘If you’re on steroids, treat your glucose like a baby-check it often, don’t ignore it, and don’t panic.’ And when it’s time to taper? That’s when you need to be extra careful. Talk to your doc before you stop anything.