Colorectal cancer is one of the most preventable cancers-if you catch it early. That’s why colonoscopy screening isn’t just a routine checkup; it’s a life-saving step for anyone 45 and older. The rules changed in 2021, and now, if you’re average risk, you should start getting screened at 45, not 50. Why? Because more young adults are being diagnosed. Rates of colorectal cancer in people under 50 have been rising by about 2% every year since the mid-90s. The good news? Finding and removing precancerous polyps during a colonoscopy can stop cancer before it starts.
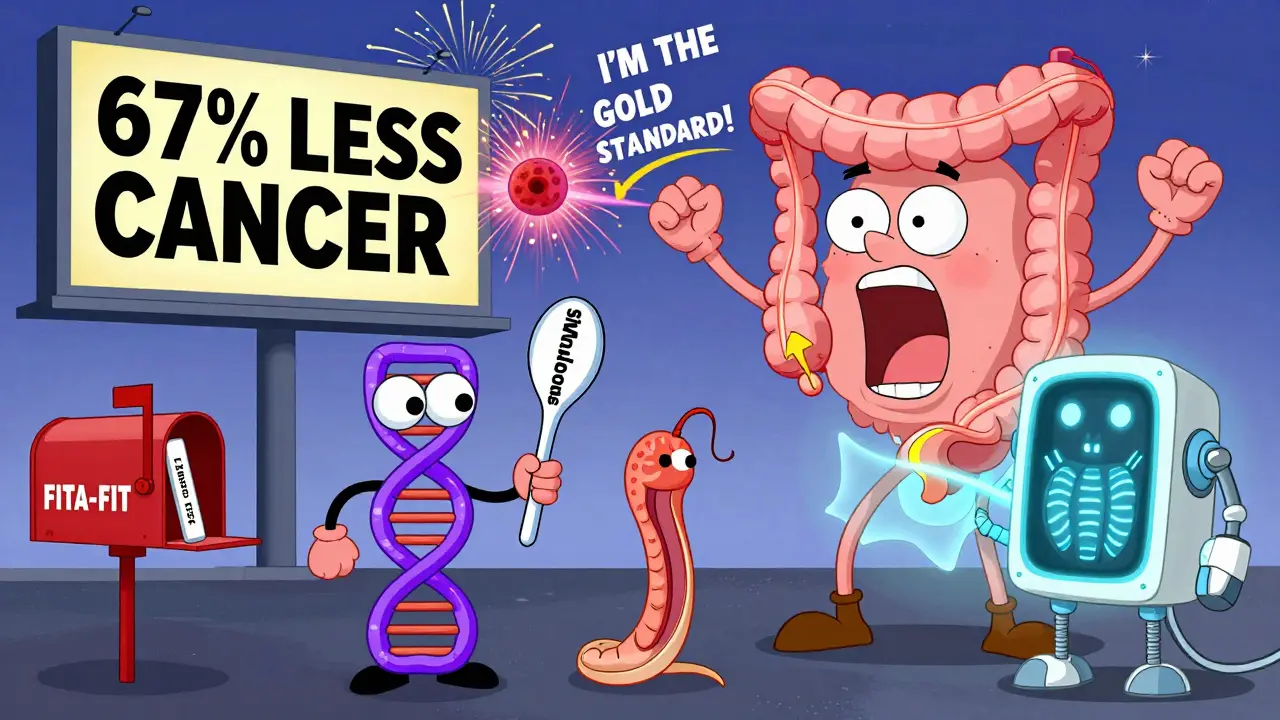
Colonoscopy: The Gold Standard for Prevention
Colonoscopy is still the most effective screening tool for colorectal cancer. It’s the only test that lets doctors see the entire colon, find polyps, and remove them right then and there. No other test can do that. Studies show it cuts colorectal cancer risk by 67% and reduces deaths by 65%. That’s not a small win-it’s huge.
The procedure itself takes about 30 minutes. You’ll be sedated, so you won’t feel anything. The real challenge? The prep. Most people say the bowel cleanse is the worst part. You’ll need to drink a large volume of liquid laxative the day before. Polyethylene glycol (PEG) solutions work best, even if they taste unpleasant. Newer low-volume options exist, but they’re less reliable. If you skip the prep or do it poorly, you risk missing polyps.
After the procedure, you’ll need someone to drive you home. Most people feel fine the next day. Complications like bleeding or perforation are rare-about 1 in every 1,000 to 1,500 colonoscopies. But when they happen, they’re serious. That’s why choosing an experienced provider matters. Look for a gastroenterologist with an adenoma detection rate (ADR) of at least 25%. Higher ADR means they’re better at spotting precancerous growths.
If your colonoscopy is clean, you won’t need another for 10 years. If you have one or two small polyps, you might need to come back in 5 to 7 years. More polyps or larger ones? You could need another in 3 years. Your doctor will give you a clear plan based on what they find.
Other Screening Options: What Works and What Doesn’t
Not everyone wants a colonoscopy. That’s okay. There are other options-but they’re not all equal.
- Fecal Immunochemical Test (FIT): You collect a stool sample at home. It checks for hidden blood, which can signal cancer or large polyps. It’s accurate (79-88% for detecting cancer), cheap, and non-invasive. But you have to do it every year. Miss a year, and you lose protection. In safety-net clinics, FIT adherence is 67%-much higher than colonoscopy’s 42%.
- Stool DNA test (sDNA-FIT): This one looks for both blood and DNA changes linked to cancer. It’s more sensitive than FIT (92% vs. 74%) but less specific. That means more false positives. If it comes back positive, you’ll still need a colonoscopy. It’s recommended every 3 years.
- Flexible sigmoidoscopy: Only examines the lower third of the colon. Less prep, no sedation. It reduces distal cancer risk by 26% and death by 28%. But it misses polyps in the upper colon. You need it every 5 years, often paired with annual FIT.
- CT colonography (virtual colonoscopy): Uses X-rays to create 3D images. No sedation, but you still need bowel prep. It can’t remove polyps. If it finds anything, you need a colonoscopy anyway. Plus, it exposes you to radiation-about the same as a chest CT.
The bottom line? Colonoscopy is the most effective. But if you’re scared, anxious, or can’t get an appointment, FIT or sDNA-FIT are valid alternatives. Just don’t skip screening altogether. The risk of dying from colorectal cancer without screening is 4 times higher than with it.
Who Needs to Start Earlier Than 45?
If you have a family history of colorectal cancer or polyps, you might need to start screening before 45. Same if you have:
- Lynch syndrome or familial adenomatous polyposis (FAP)
- Chronic inflammatory bowel disease (Crohn’s or ulcerative colitis)
- A personal history of colorectal cancer or polyps
In these cases, colonoscopy is the only recommended option. For Lynch syndrome, screening often starts at 20-25 or 2-5 years before the youngest case in your family. If you’re African American, you’re at higher risk-20% higher incidence and 40% higher death rate. That’s why experts recommend starting at 45, even if you have no family history.
People over 75? Screening becomes more individualized. If you’re healthy and have a life expectancy of more than 10 years, you can keep going. If you’re frail or have other serious conditions, screening may do more harm than good. Talk to your doctor.
What Happens If Cancer Is Found?
If a colonoscopy finds cancer, the next step is staging. That means figuring out how far it’s spread. This is done with CT scans, MRIs, and sometimes PET scans. The stage determines treatment.
Stage I: Cancer is only in the inner layers of the colon. Surgery alone is often enough. 90%+ survival rate.
Stage II: Cancer has grown into the outer layers but hasn’t reached lymph nodes. Surgery is still the main treatment. Some patients get chemotherapy if there are high-risk features like poor cell differentiation or blocked bowel.
Stage III: Cancer has spread to nearby lymph nodes. Here, chemotherapy is standard after surgery. The goal? Kill any hidden cancer cells.
Stage IV: Cancer has spread to distant organs like the liver or lungs. Surgery may still be used to remove tumors if possible. But chemotherapy becomes the main tool.
Chemotherapy Regimens for Colorectal Cancer
Chemotherapy for colorectal cancer isn’t one-size-fits-all. It’s tailored to stage, genetics, and overall health.
For stage III and some stage II cancers, the most common regimens are:
- FOLFOX: A combination of 5-fluorouracil (5-FU), leucovorin, and oxaliplatin. Given every 2 weeks for 6 months. Common side effects: nerve damage (tingling in hands/feet), fatigue, nausea.
- CAPOX (XELOX): Capecitabine (oral pill) and oxaliplatin. Also given every 3 weeks. Same effectiveness as FOLFOX, but you take one drug at home. Less frequent clinic visits.
- 5-FU + leucovorin: Older regimen. Used less now, but still an option for people who can’t tolerate oxaliplatin.
For stage IV cancer, treatment is longer-term. Often, doctors add targeted drugs:
- Bevacizumab (Avastin): Blocks blood vessel growth to tumors. Used with chemo.
- Cetuximab or panitumumab: Used only if the tumor has a wild-type RAS gene (tested via biopsy). These drugs work better in left-sided colon cancers.
- Trifluridine/tipiracil (Lonsurf) or regorafenib (Stivarga): Used later, when other chemo options fail.
Side effects vary. Nerve damage from oxaliplatin can last months or years. Diarrhea, low blood counts, and fatigue are common. But many people tolerate these regimens well. Your oncologist will monitor you closely and adjust doses as needed.
Genetic testing matters. If your tumor has MSI-H or dMMR, immunotherapy like pembrolizumab may be an option-even for advanced cases. That’s a game-changer for a small group of patients.

Barriers to Screening and How to Overcome Them
Despite all the evidence, only 67% of adults 50-75 are up to date with screening. Why? Cost, fear, lack of access, or just putting it off.
Uninsured? You may qualify for free or low-cost screening through state programs. Medicare covers colonoscopy every 10 years (or every 5 if you’re high risk). Medicaid coverage varies by state.
Can’t get an appointment? Wait times in rural areas can be 60+ days. Patient navigators-staff who help you schedule, prep, and follow up-can cut delays by 35%. Ask your clinic if they have one.
Language or cultural barriers? Stool tests often work better here. They’re easier to explain, less intimidating, and can be done at home. A 2021 study found Hispanic patients were 9% more likely to complete FIT than colonoscopy.
Don’t wait for symptoms. By the time you feel pain, bloating, or blood in stool, the cancer may already be advanced. Early-stage colorectal cancer often has no symptoms at all.
What’s Next for Screening?
Researchers are working on blood tests that could detect colorectal cancer early. The Guardant SHIELD test showed 83% sensitivity in a 2023 trial. It’s not ready for prime time yet, but it’s promising. AI tools like GI Genius, already FDA-approved, help doctors spot polyps during colonoscopy-increasing detection by 14%.
Future guidelines may use risk scores-combining genetics, diet, weight, and lifestyle-to personalize screening intervals. Instead of everyone getting a colonoscopy every 10 years, low-risk people might go every 15, while high-risk people get one every 3.
The goal? Prevent more cancers, catch more early, and make screening easier for everyone.
At what age should I start colonoscopy screening for colorectal cancer?
If you’re at average risk, start at age 45. This is the current standard from the U.S. Preventive Services Task Force, the American Cancer Society, and the American College of Gastroenterology. If you have a family history of colorectal cancer, polyps, or a genetic syndrome like Lynch syndrome, you may need to start earlier-sometimes as young as 20 to 25. Talk to your doctor about your personal risk.
Is colonoscopy the only way to screen for colorectal cancer?
No, but it’s the most effective. Other options include annual FIT stool tests, stool DNA tests every 3 years, flexible sigmoidoscopy every 5 years, and CT colonography every 5 years. But only colonoscopy lets your doctor remove polyps during the test. If any other test comes back positive, you’ll still need a colonoscopy to confirm and treat.
What are the most common chemotherapy regimens for colorectal cancer?
For stage III cancer, FOLFOX (5-FU, leucovorin, oxaliplatin) and CAPOX (capecitabine and oxaliplatin) are the most common. Both are given for 6 months after surgery. For advanced (stage IV) cancer, doctors often add targeted drugs like bevacizumab or cetuximab. The choice depends on tumor genetics, your health, and side effect tolerance.
Can I avoid chemotherapy if my cancer is caught early?
Yes, if your cancer is stage I, surgery alone is usually enough. For stage II, chemo isn’t always needed-it depends on whether the tumor has high-risk features like poor differentiation or bowel obstruction. Stage III almost always requires chemo after surgery to kill any hidden cancer cells.
How often do I need to get screened after a normal colonoscopy?
If your colonoscopy finds no polyps or only 1-2 small, low-risk adenomas, you’ll likely wait 10 years for your next one. If you have 3-10 polyps, or any larger than 1 cm, you’ll need another in 3 to 5 years. If you have more than 10 polyps, you may need one in 1 year. Always follow your doctor’s specific recommendation.
Why is colorectal cancer rising in younger adults?
The exact reasons aren’t clear, but experts point to rising rates of obesity, processed food diets, sedentary lifestyles, and changes in gut bacteria. There’s no single cause, but the trend is real: since 1994, colorectal cancer rates in people under 50 have increased by over 50%. That’s why screening now starts at 45.

