When you're taking carbamazepine for epilepsy or nerve pain, the last thing you want is for your medication to stop working - or worse, to cause new side effects. But if your pharmacy switches your prescription from one generic version to another, that’s exactly what can happen. Carbamazepine isn’t just any generic drug. It’s one of the most tricky ones out there, and here’s why.
Why carbamazepine is different
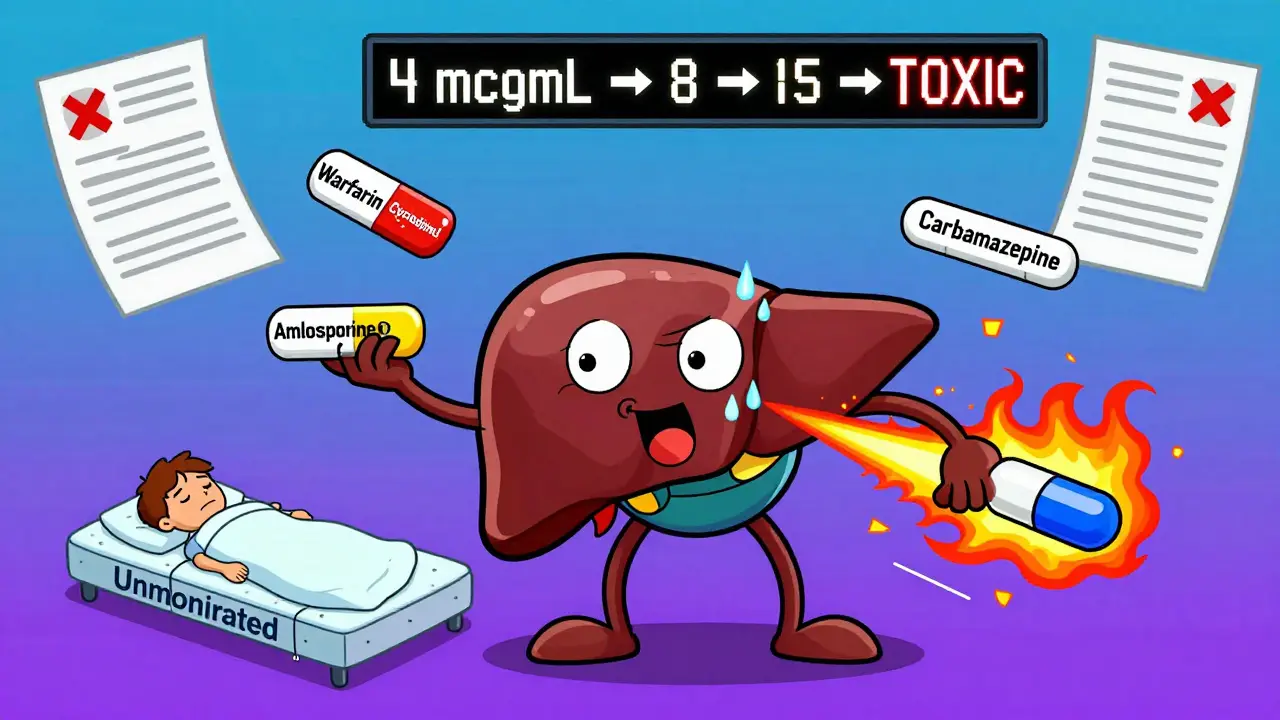
Carbamazepine was first approved in 1974 under the brand name Tegretol. Today, over 30 different generic versions are available in the U.S. alone. On paper, they’re all the same: same active ingredient, same dose, same FDA approval. But in real life, they’re not interchangeable. The reason? Carbamazepine has a narrow therapeutic index (NTI). That means the difference between a dose that works and one that’s dangerous is tiny. The target blood level is 4-12 mcg/mL. Go below 4, and seizures might come back. Rise above 12, and you risk dizziness, nausea, or even toxic reactions.Adding to the complexity, carbamazepine doesn’t just sit in your body - it changes how your body processes other drugs. It’s a powerful enzyme inducer, meaning it cranks up your liver’s CYP3A4 enzyme system. This enzyme breaks down about half of all prescription medications. So if you’re on carbamazepine, your body starts clearing out other drugs faster than normal. That includes blood thinners like warfarin, heart meds like amlodipine, immunosuppressants like cyclosporine, and even some HIV drugs. If you’re not monitored, these drugs can drop to ineffective levels. One patient on warfarin might suddenly develop a blood clot. Another on tacrolimus after a transplant could reject their organ.
Autoinduction: the drug that speeds up its own breakdown
What makes carbamazepine especially dangerous is that it induces its own metabolism. This is called autoinduction. When you first start taking it, your body doesn’t break it down quickly. But within 48 to 72 hours, your liver starts producing more enzymes. By two to three weeks, you’re clearing carbamazepine up to 50% faster than when you started. That means your blood levels drop - even if you take the same dose every day.Many patients think they’re fine because their first blood test was normal. But if you don’t retest after a few weeks, you could be underdosed without knowing it. A 2022 study in the Journal of Clinical Pharmacy and Therapeutics found that 65-75% of epilepsy patients on carbamazepine need regular blood tests just to stay stable. And if you switch generics? That reset clock can start all over again.
Generics aren’t created equal
All generic carbamazepine must prove bioequivalence - meaning their absorption in healthy volunteers falls within 80-125% of the brand drug. Sounds fair, right? But here’s the catch: those studies are done in 24-36 healthy people, not in patients with epilepsy, liver disease, or who are taking 5 other medications. Real patients are more complex.A 2018 study in Epilepsia followed 327 patients who were switched between different generic brands. Over 12% had breakthrough seizures or new side effects. Nearly 8% ended up in the emergency room. Why? Because even small differences in how the tablet dissolves or how the beads release the drug can throw off absorption - especially when carbamazepine’s metabolism is already unstable.
Extended-release versions like Carbatrol or Tegretol XR are supposed to be more stable. But even here, problems arise. One patient in a 2023 study had gastroparesis - a condition that slows stomach emptying. The generic version they were switched to had larger beads that didn’t dissolve properly in their stomach. Their levels dropped 30%. They started having daily seizures.
Gender, genetics, and race matter
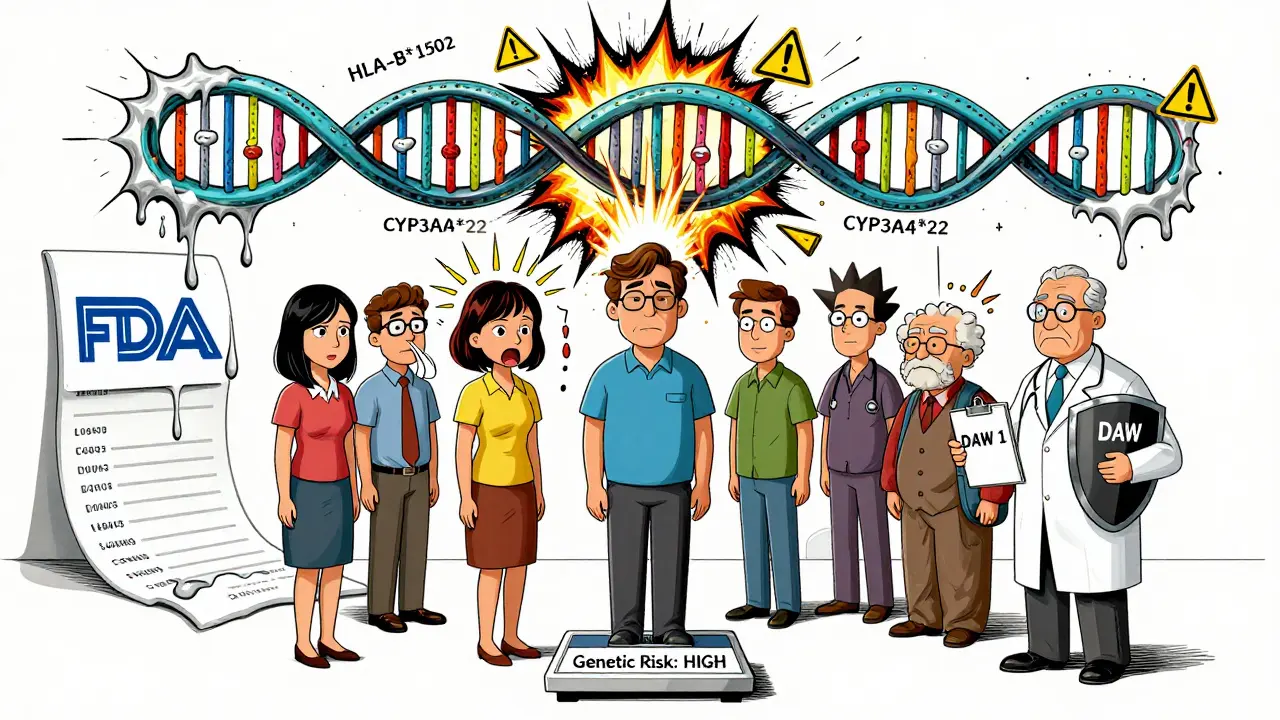
Your body doesn’t process carbamazepine the same way as someone else’s. Women tend to metabolize it faster than men due to higher CYP3A4 activity. A 2021 study in Pharmacogenetics and Genomics found women had 20-25% higher enzyme activity. That means women often need slightly higher doses - but only if their levels are checked.And then there’s genetics. People of Asian descent carry the HLA-B*1502 gene variant in up to 15% of cases. If you have it and take carbamazepine, your risk of developing Stevens-Johnson Syndrome - a life-threatening skin reaction - jumps 10-fold. The FDA recommends testing for this gene before starting carbamazepine in Asian populations. Many doctors skip this step. Don’t. It’s not optional.
Even within the same population, over 17 genetic variations affect how carbamazepine is broken down. One variant, CYP3A4*22, reduces metabolism by 25%. Someone with this gene might need a dose 25% lower than average. Without testing, they’re at risk of toxicity.
What you should do
If you’re on carbamazepine, here’s what actually works:- Ask for the same manufacturer every time. If your prescription says “Tegretol XR,” insist on that brand. If you’re on generic, ask your pharmacist which company makes it. Write it down. Stick with it.
- Get your blood tested. Test before any switch, 7-10 days after, and again at 4 weeks. If your level changes by more than 15%, your dose needs adjustment.
- Use “dispense as written” (DAW 1). Tell your doctor to write this on your prescription. It legally prevents the pharmacy from swapping generics without your consent.
- Don’t assume generics are safe. The FDA’s own data shows 28.6% of all reported generic-related issues involve carbamazepine - second only to lamotrigine.
- Know your risk factors. If you’re Asian, female, on multiple meds, or have liver issues, you’re at higher risk. Talk to your neurologist about therapeutic drug monitoring.
What’s being done
The FDA now classifies carbamazepine as a high-priority NTI drug. Their 2023 draft guidance requires new testing methods - including in vitro-in vivo correlation (IVIVC) modeling - to better predict how different formulations behave in real patients. The European Medicines Agency already requires steady-state bioequivalence studies for all NTI drugs, meaning they test after the drug has stabilized in the body, not just after a single dose.Researchers are building precision dosing tools. A toolkit from the American Epilepsy Society, coming in late 2024, will help doctors adjust doses based on age, sex, weight, and other medications. And by 2030, experts predict genetic testing will be standard before prescribing carbamazepine.


Comments
Lakisha Sarbah
February 7, 2026 AT 14:33Marcus Jackson
February 7, 2026 AT 20:43Patrick Jarillon
February 8, 2026 AT 09:07Ritu Singh
February 9, 2026 AT 21:09Mark Harris
February 10, 2026 AT 22:14Mayank Dobhal
February 12, 2026 AT 15:34Joey Gianvincenzi
February 14, 2026 AT 02:25Natasha Bhala
February 15, 2026 AT 22:02