Bridging Therapy Risk Calculator
Assess Your Bridging Need
This tool helps determine if bridging therapy is medically necessary based on current guidelines. Select your specific conditions below.
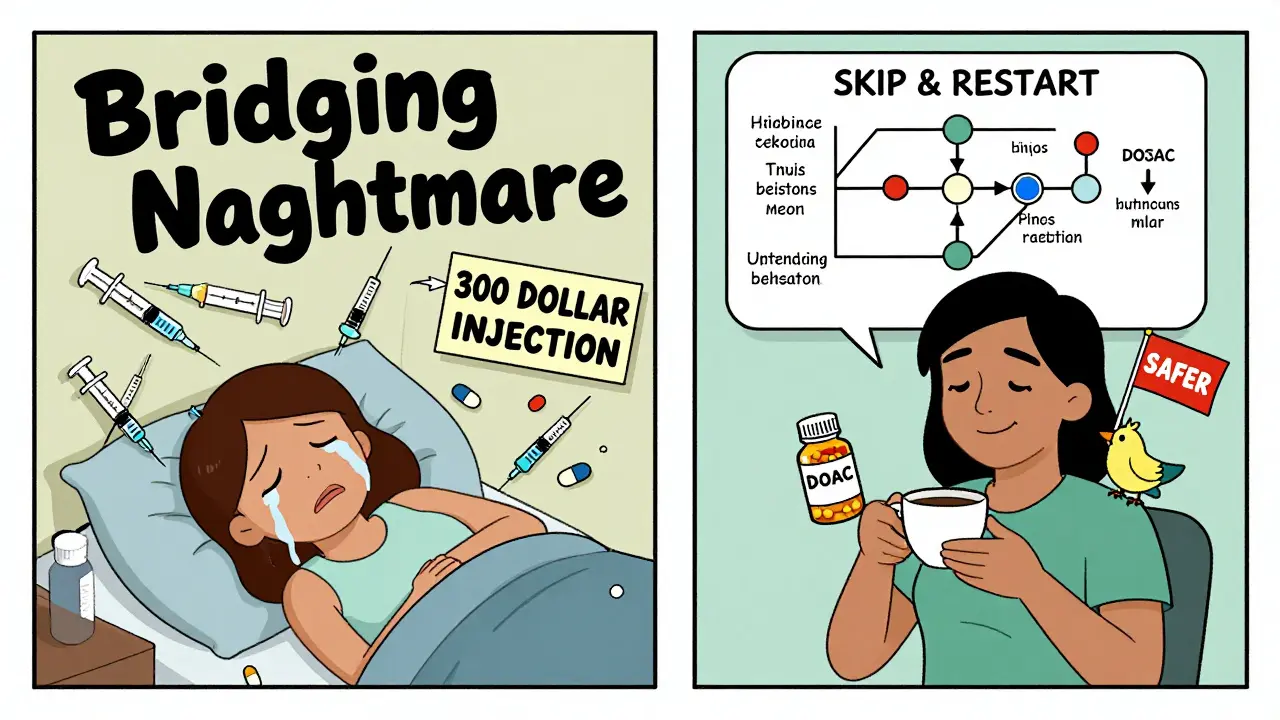
Switching between blood thinners isn’t as simple as stopping one pill and starting another. For many people on long-term anticoagulation, a temporary pause in treatment is needed - whether for surgery, a dental procedure, or an injury. But stopping your blood thinner without a plan can be dangerous. Too little protection, and you risk a stroke or clot. Too much, and you could bleed internally. That’s where bridging therapy comes in. But here’s the twist: for most people today, bridging isn’t needed at all.
What Is Bridging Therapy, Really?
Bridging therapy means using a fast-acting injectable blood thinner - like low molecular weight heparin (LMWH) - to temporarily replace your regular blood thinner while it’s paused. It’s meant to keep your blood from clotting during the gap. This used to be routine. If you were on warfarin and needed a knee replacement, your doctor would likely stop warfarin, start you on daily injections, and then restart warfarin after surgery. But that’s not the norm anymore. A major study in 2015 called the BRIDGE trial showed something shocking: patients who were bridged had more major bleeding - 2.3% - compared to those who didn’t bridge at all, which was just 1%. And there was no drop in strokes or clots. In fact, some patients bled more because of the extra injections. Now, guidelines have changed. Bridging isn’t a default. It’s a last resort.When Is Bridging Actually Necessary?
Not everyone needs it. In fact, only about 10-15% of people on blood thinners today even qualify. Bridging is only recommended if you’re at very high risk for clots. That means:- You have a mechanical heart valve in the mitral position (the left side of the heart)
- You had a blood clot in your leg or lung within the last 3 months
- You have atrial fibrillation with a CHA₂DS₂-VASc score of 5 or higher (that’s a scoring system doctors use to measure stroke risk)
Why DOACs Changed Everything
Ten years ago, warfarin was the only option. It’s slow to start, slow to wear off, and needs weekly blood tests to check your INR. That’s why bridging was common - you couldn’t just skip a few doses and expect safety. Now? Direct oral anticoagulants (DOACs) like apixaban (Eliquis), rivaroxaban (Xarelto), and dabigatran (Pradaxa) are used in 75% of new prescriptions. Why? Because they’re predictable. They work within hours. They leave your system in 1-2 days. No blood tests. No injections. For DOAC users, bridging is almost never needed. Here’s how it works:- If you’re on apixaban and need a procedure, you skip your dose 2 days before. Restart it 12-24 hours after.
- For dabigatran, stop 2-3 days before if you have normal kidney function. Restart after 24 hours.
- No heparin shots. No bridges. Just timing.

How Bridging Works If You’re Still on Warfarin
If you’re one of the few still on warfarin and your doctor says you need bridging, here’s what to expect:- Stop warfarin 5-6 days before your procedure. This lets your INR drop safely.
- Start LMWH (like enoxaparin) 3 days before. Usually a daily injection under the skin.
- Stop the LMWH 24 hours before surgery. This reduces bleeding risk during the procedure.
- After surgery, restart LMWH 12-24 hours later if bleeding is controlled.
- Restart warfarin the same day, often at 15-20% higher than your usual dose.
- Check your INR in 3-4 days to make sure it’s back in range.
What About Switching Between Blood Thinners?
Sometimes, people need to switch from warfarin to a DOAC - or vice versa. This isn’t bridging, but it still needs care. If switching from a DOAC to warfarin:- Stop the DOAC.
- Start warfarin right away, along with a short course of LMWH.
- Keep the LMWH going until your INR hits 2.0 or higher.
- Then stop the injections.
- Stop warfarin when your INR is below 2.0.
- Start the DOAC the next day.
- No bridging needed.
What Doctors Are Saying Now
The old thinking was: better safe than sorry. So we bridged everyone. But evidence changed that. The BRIDGE trial, led by Dr. James Douketis, showed bridging increased bleeding without reducing clots. The PERIOP2 trial in 2020 confirmed it. The American College of Cardiology now says: “Physician preferences for routine bridging may be too aggressive.” Most guidelines today agree: Don’t bridge unless you absolutely must. For atrial fibrillation patients without mechanical valves or recent clots? Skip the injections. Just pause the pill, wait a few days, restart. For mechanical valve patients? Yes, bridge. But even then, some centers are testing whether low-dose prophylactic heparin is enough - not full therapeutic doses.What You Should Do
If you’re on a blood thinner and have a procedure coming up:- Don’t assume you need bridging. Ask your doctor: “Am I at high enough risk for a clot to justify the bleeding risk from injections?”
- If you’re on a DOAC, ask if you even need to stop it - many minor procedures don’t require stopping at all.
- If you’re on warfarin, get your INR checked 5-7 days before surgery. If it’s low, you might not need bridging.
- Make sure your surgeon and pharmacist are on the same page. Miscommunication is a leading cause of errors.
- Write down your plan: what to stop, when, and when to restart. Keep a copy with you.
The Bottom Line
Bridging therapy was born out of necessity. But modern medicine has moved past it. For most people, the risks of bridging outweigh the benefits. The goal isn’t to keep you perfectly protected at all times - it’s to avoid harm. And sometimes, doing less is safer. If you’re on warfarin and have high-risk features, bridging still has a place. But if you’re on a DOAC, or if your stroke risk is moderate? You probably don’t need it. Ask questions. Push for evidence. Your body will thank you.Do I always need to stop my blood thinner before surgery?
No. Many minor procedures - like dental cleanings, skin biopsies, or cataract surgery - don’t require stopping your blood thinner at all. For DOAC users, especially, the risk of bleeding is often lower than the risk of stopping. Always ask your doctor or surgeon if stopping is truly necessary.
Can I switch from warfarin to a DOAC without bridging?
Yes. When switching from warfarin to a DOAC, you stop warfarin when your INR is below 2.0, then start the DOAC the next day. No injections or bridging are needed. This is one reason DOACs are now preferred - they’re simpler and safer to transition.
Why is LMWH used for bridging instead of other injectables?
Low molecular weight heparin (LMWH) like enoxaparin is preferred because it’s predictable, given once or twice daily by injection, and doesn’t need blood monitoring. Unfractionated heparin requires constant IV infusion and lab checks, making it impractical for outpatient bridging. Fondaparinux is rarely used because it lasts too long - 36-48 hours - increasing bleeding risk.
What if I miss a bridging injection?
Missing one injection increases your clot risk, especially if you’re high-risk. If you miss a dose, call your doctor immediately. Do not double up. Depending on timing, they may advise you to skip the rest of the course or adjust your schedule. Never guess - always get professional advice.
Is bridging therapy covered by insurance?
In most cases, yes - but only if it’s medically necessary. Insurance companies now require proof of high thrombotic risk before approving bridging. If your doctor can’t justify it with your CHA₂DS₂-VASc score or history of clots, coverage may be denied. Many patients pay out of pocket, especially in the U.S., where a 7-day course can cost $300-$500.

