What You Need to Know About Bipolar Disorder Medications
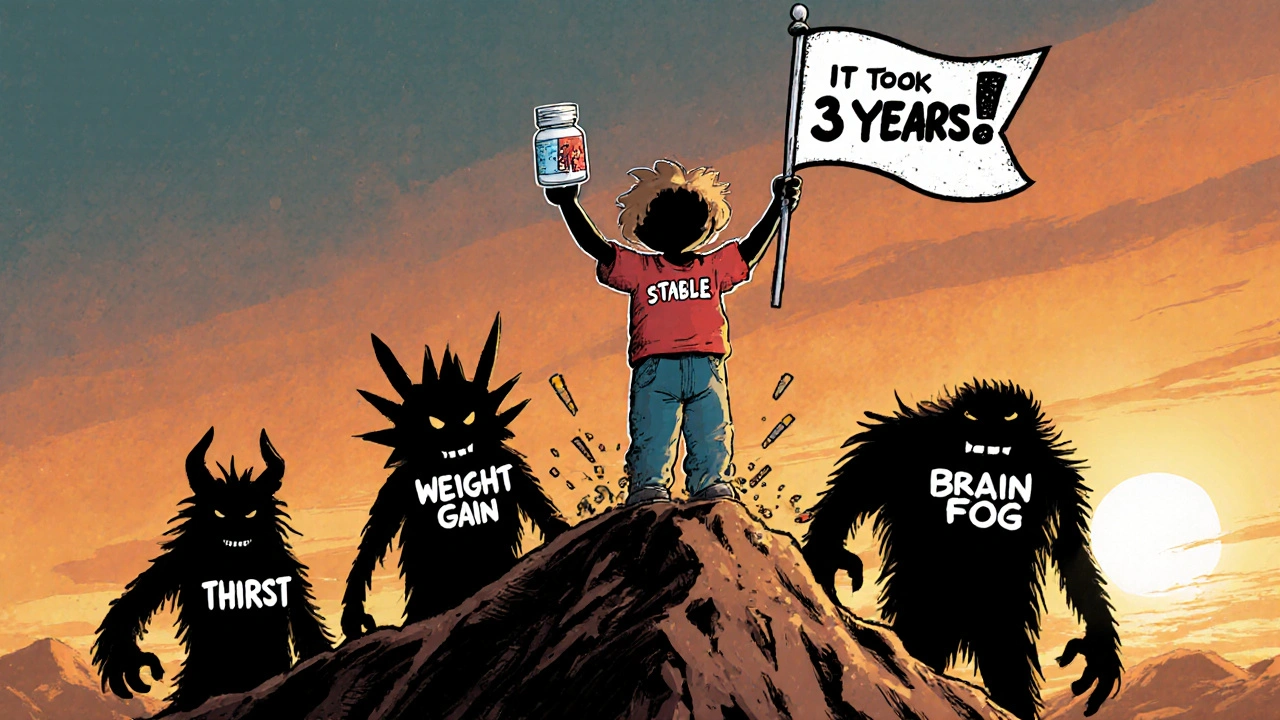
Living with bipolar disorder means dealing with extreme mood swings-sometimes crashing into deep depression, other times racing into mania. Medications like mood stabilizers and antipsychotics are the backbone of treatment, but they’re not magic pills. They work best when you understand how they act, what side effects to expect, and how to work with your doctor to find the right balance. Many people stop taking their meds because of weight gain, constant thirst, or brain fog-not because the drugs don’t work. The truth is, finding the right combination can take months, even years. But when it clicks, it can mean the difference between surviving and truly living.
Mood Stabilizers: The Foundation of Long-Term Control
Lithium has been the gold standard since the 1970s, and for good reason. It doesn’t just calm mania-it cuts suicide risk by 80% compared to no treatment. But it’s not simple. You need regular blood tests to keep levels between 0.6 and 1.0 mmol/L. Too low, and it won’t help. Too high, and you risk tremors, confusion, or even seizures. Most people on lithium notice increased urination and thirst right away. Some drink three liters of water a day just to keep up. Weight gain is common too-10 to 15 pounds in the first year isn’t unusual.
Valproate and carbamazepine are alternatives, especially if lithium causes too many side effects. But valproate carries serious risks for women of childbearing age-it can cause birth defects. Lamotrigine is different. It’s the best mood stabilizer for preventing depressive episodes, with a 47% response rate. But it comes with a scary warning: a 10% chance of a serious skin rash. That’s why doctors start you on a tiny dose and increase it slowly over weeks.
Antipsychotics: Fast Relief, But Heavy Costs
If you’re in the middle of a manic episode, antipsychotics like quetiapine (Seroquel) or olanzapine can bring calm faster than lithium. Some people feel better in just a few days. But there’s a trade-off. Quetiapine causes drowsiness in 60-70% of users. Olanzapine leads to major weight gain-around 4.6 kilograms in just six weeks. That’s not just cosmetic. It raises your risk of type 2 diabetes by 20-30%. Aripiprazole and risperidone are options too, but they can cause restlessness (akathisia) or muscle stiffness.
These drugs aren’t just for mania. Quetiapine is also FDA-approved for bipolar depression. In studies, over half of people on quetiapine saw improvement, compared to just over 30% on placebo. But real-world experience is harsher. On patient forums, 68% report weight gain averaging 22 pounds. One person wrote, “I took it to stop the screaming depression, but now I can’t fit into my clothes. Is it worth it?” For many, the answer is yes-but only if they’re monitored closely.
Combining Medications: More Power, More Problems
When one drug isn’t enough, doctors often add a second. Combining a mood stabilizer with an antipsychotic boosts response rates to 70% in tough cases. But side effects pile up. Weight gain, dizziness, metabolic changes-they don’t just add up, they multiply. About 25-30% more people report severe side effects when on both types of meds.
That’s why doctors don’t jump to combinations right away. They start with one, wait to see how you respond, and only add another if needed. The goal isn’t to throw everything at the wall. It’s to find the smallest effective mix. Some people do well on lithium alone. Others need lamotrigine and low-dose quetiapine. It’s personal.

What About Antidepressants?
It’s tempting to add an SSRI like fluoxetine when you’re stuck in depression. But here’s the catch: antidepressants can flip you into mania. About 10-15% of people with bipolar disorder experience this switch. Some experts, like Dr. Gary Sachs from Harvard, say the risk is too high. Others, like Dr. David Miklowitz at UCLA, believe they’re safe if paired with a mood stabilizer.
The consensus? Never use an antidepressant alone. If you need one, it should be short-term and always paired with lithium, lamotrigine, or an antipsychotic. Even then, watch for signs of mania-racing thoughts, less sleep, impulsive spending. If you notice them, call your doctor immediately.
Monitoring and Managing Side Effects
Medication management isn’t just about taking pills. It’s about tracking your body. Every three months, you should get checked for:
- Weight and waist size (over 40 inches for men, 35 for women signals risk)
- Fasting blood sugar and cholesterol
- Thyroid and kidney function (especially if on lithium)
Many people don’t realize their fatigue or brain fog is linked to their meds. A simple blood test can reveal if your lithium level is creeping up. If you’re on quetiapine and gaining weight, metformin can help. It’s not a cure, but it can slow the gain and lower diabetes risk.
Also, avoid NSAIDs like ibuprofen or naproxen if you’re on lithium. They can spike lithium levels and cause toxicity. Even a few days of painkillers can be dangerous.
Real Stories: What Patients Say
Reddit and PatientsLikeMe are full of raw, honest stories. One person said, “Lithium gave me constant thirst. I was peeing every hour. I switched to lamotrigine-and then couldn’t sleep for weeks.” Another wrote, “After three failed meds, lithium finally worked. I gained 15 pounds, but I haven’t had a suicidal episode in two years. That’s worth it.”
Some find relief with newer options. Lumateperone (Caplyta), approved in 2023, helps with depression without the weight gain. Long-acting injectables like Abilify Maintena mean you only need one shot a month-no daily pills to forget.
What’s Changing in 2025?
Genetic testing is becoming more common. Companies like Genomind test your DNA to predict how you’ll respond to certain drugs. If you’re a slow metabolizer of CYP2D6, you might need half the dose of a common antipsychotic. This isn’t sci-fi-it’s already helping 30% of people avoid trial-and-error.
By 2027, experts predict most bipolar treatments will include some form of personalized testing. Digital tools like reSET-BD, a smartphone app that tracks mood and medication adherence, are showing promise too. In trials, users had 22% fewer relapses.
When to Call Your Doctor
You don’t have to suffer in silence. Call your psychiatrist if you notice:
- Shaky hands, slurred speech, or dizziness (possible lithium toxicity)
- Sudden weight gain, extreme thirst, or frequent urination
- Insomnia, agitation, or racing thoughts (signs of mania)
- A rash that spreads or blisters (stop lamotrigine immediately)
Don’t wait for your next appointment. These are red flags. Your doctor needs to know right away.
Final Thoughts: It’s a Journey, Not a Fix
There’s no one-size-fits-all solution for bipolar disorder. What works for one person might fail for another. Lithium isn’t perfect, but it’s still the most proven tool for long-term safety. Antipsychotics bring fast relief but come with heavy side effects. The key is patience, communication, and consistent monitoring.
Most people don’t find the right mix on the first try. That’s normal. It took three years for one woman I spoke with to land on lamotrigine plus a low dose of aripiprazole. Now she’s working full-time, traveling, and sleeping through the night. She still takes meds daily. But she’s not just surviving-she’s living.
Can you treat bipolar disorder without medication?
Therapy, routine, and lifestyle changes help-but they’re not enough on their own for most people. Bipolar disorder is a brain chemistry condition. Medications like mood stabilizers and antipsychotics directly target those imbalances. Without them, episodes become more frequent and severe. Some people use supplements like omega-3s or mindfulness, but studies show they only support-not replace-medication.
How long does it take for mood stabilizers to work?
Lithium and valproate usually take 1 to 3 weeks to reduce mania. Lamotrigine works slower-it can take 6 to 12 weeks to ease depression. Antipsychotics like quetiapine often show improvement in 5 to 7 days. Patience is key. Doctors start low and go slow to avoid side effects. Rushing the dose increase can make things worse.
Do antipsychotics make you gain weight permanently?
Not always, but it’s common. Olanzapine and quetiapine are the worst offenders. Some people gain 10-20 pounds in the first few months. But weight gain isn’t inevitable. Eating a balanced diet, exercising regularly, and using metformin can help. Some switch to newer antipsychotics like lumateperone or lurasidone, which have minimal weight gain. The goal isn’t to avoid meds-it’s to find ones that work without wrecking your health.
Is lithium dangerous for your kidneys?
Long-term lithium use can affect kidney function, but it’s rare if you’re monitored. Blood tests every 3 months check your creatinine and eGFR levels. If kidney function drops, your doctor can lower your dose or switch you. Most people on lithium for 10+ years have normal kidney function. The risk is higher if you’re dehydrated or take NSAIDs. Stay hydrated, avoid ibuprofen, and get tested regularly.
Can you stop taking bipolar meds if you feel better?
No. Stopping abruptly can trigger a severe relapse-sometimes worse than before. Even if you’ve been stable for a year, your brain still needs the chemical support. Tapering off should only happen under close medical supervision, over months or even years. Many people who quit meds end up back in the hospital. Stability isn’t the same as being cured.
Are generic mood stabilizers as good as brand names?
Yes, for lithium, valproate, and carbamazepine. These generics are identical in active ingredients and work just as well. The problem is with antipsychotics-some brand names have slightly different formulations that affect absorption. But for most people, generics are safe and cost far less. Lithium carbonate costs $4 to $40 a month. Brand-name antipsychotics like Vraylar can hit $1,200. Save money where you can.
What’s the best way to remember to take your meds?
Use a pill organizer with morning and night slots. Set phone alarms labeled “Lithium” or “Quetiapine.” Link taking meds to a daily habit-like brushing your teeth or eating breakfast. Apps like Medisafe or MyTherapy send reminders and track adherence. Some long-acting injectables (like Abilify Maintena) only need monthly shots, which removes the daily pressure. Consistency beats perfection.
Can bipolar meds affect your sex life?
Yes. Sexual side effects-low desire, trouble with arousal, delayed orgasm-are common with almost all these drugs. Studies show over half of patients report this. It’s not talked about enough. Talk to your doctor. Sometimes switching meds helps. Lowering the dose can too. There are also medications like bupropion that can help counteract this side effect without triggering mania.


Comments
Jessica Chambers
November 14, 2025 AT 12:05Shyamal Spadoni
November 15, 2025 AT 02:01Ogonna Igbo
November 16, 2025 AT 04:46BABA SABKA
November 16, 2025 AT 13:05Chris Bryan
November 17, 2025 AT 21:39Jonathan Dobey
November 18, 2025 AT 01:55ASHISH TURAN
November 18, 2025 AT 05:20Ryan Airey
November 19, 2025 AT 00:17Hollis Hollywood
November 20, 2025 AT 07:51Aidan McCord-Amasis
November 21, 2025 AT 04:26Adam Dille
November 21, 2025 AT 15:51Katie Baker
November 22, 2025 AT 13:22